
Medical oncologist Darren Feldman and the rest of Memorial Sloan Kettering's testicular cancer team offer expert care and the latest treatment options.
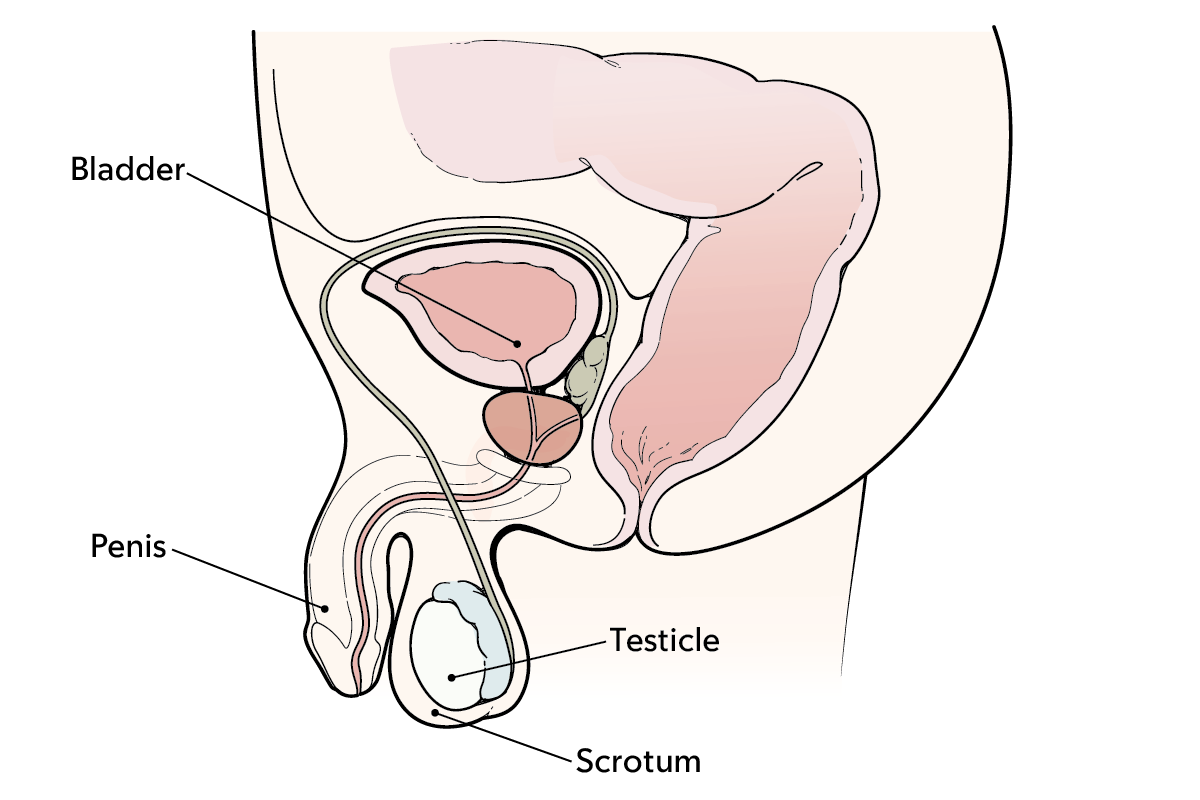
A testicle, scrotum, and penis.
Testicles (testes) are located below your penis. They are 2 small, egg-shaped glands that make and store sperm. The loose skin around them is called the scrotum.
Testicles have many special cells. They contain germ cells that make sperm, and other cells that make testosterone.
Testicular (tes-TIH-kyoo-ler) cancer is not a common disease. Each year, only about 9,000 people in the United States get testicular cancer. Many of them between the ages of 15 and 35. Most cases of testicular cancer can be cured.
Who is this disease guide for?
You’re waiting to learn if you have cancer
This guide gives you information about testicular cancer so you’re better prepared.
You want a second opinion
This guide explains new treatments. Learning about them can help you decide if you want a second opinion. MSK’s testicular cancer experts offer second opinions about both diagnosis and treatment options, no matter where you live.
You’re worried about your current treatment plan
This guide can help you learn about other treatment options. MSK experts only use the latest treatments for testicular cancer, some only offered at MSK and very few other hospitals.
You’re worried about your genetic risk for cancer
This guide can help you learn about your risk for cancer. We offer cancer genetic risk assessments to see if you’re at higher risk for some forms of cancer.
You’re a caregiver to someone who has cancer
This guide has information about how to support a loved one who has cancer, even if they’re not an MSK patient. At MSK, supporting caregivers is as important as caring for people with cancer.
Types of testicular tumors
About 95 out of every 100 testicular cancers start in germ cells. These are cells in the testicles that make sperm.
These tumors often start in the testicles. But they also can start in the abdomen (belly), chest, or other areas of the body. This can happen even if there’s no sign of cancer in or near the testicles.
Two of the most common germ cell tumors are seminoma (SEH-mih-NOH-muh) and nonseminoma.
Seminomas make up about half of all germ cell tumors. They often grow slowly. Most early-stage seminoma can be cured by removing the testicle during surgery. You may not need other treatment, because this cancer is less likely to metastasize (spread).
Nonseminomas are often more aggressive than seminomas. They’re more likely to spread beyond the testicle. You may need chemotherapy, surgery, or both to cure this cancer.
About 5 out of every 100 testicular cancers start in stromal cells. These cells make testosterone or support the growth of sperm. Testicular stromal tumors are often benign (not cancer).
Risk factors for testicular cancer
Testicular cancer is not linked to any habits, activities, or lifestyles.
But there are 2 important risk factors that can raise your chance of getting the disease.
- An undescended testicle. Testicles descend (drop down) from the abdomen to the scrotum before you’re born. If you were born with a testicle that did not descend, you have a greater risk of testicular cancer. That’s true even if you had surgery to fix the problem.
- You already had testicular cancer. If you had cancer in 1 of your testicles, you’re more likely to get cancer in the other one. However, the lifetime risk of this happening is low (1% to 2%). Out of every 100 people who had testicular cancer, only 1 or 2 will get it again.
There have been new advances in the diagnosis and treatment of this cancer. Most people can survive the disease, especially if the tumor is found at an early stage.
Why should I choose Memorial Sloan Kettering to treat testicular cancer?
MSK’s team of testicular cancer experts
Doctors at the Sidney Kimmel Center for Prostate and Urologic Cancers at Memorial Sloan Kettering Cancer Center (MSK) are among the nation’s most experienced in treating testicular cancer. They are part of a team that was ranked #1 in the nation for Urology Cancer Care this year by U.S. News & World Report. Each year, MSK’s testicular cancer care team sees about 500 people newly diagnosed with this disease while caring for thousands.
New ways to diagnose and treat testicular cancer
We use the latest imaging and laboratory tests to diagnose the cancer and learn more about the tumor.
Our specialists work as a team to plan the best treatment for you. For early-stage tumors, this often includes surgery. You also may have chemotherapy if the tumor is more advanced.
The latest testicular cancer research and clinical trials
MSK is a major research institution. During your treatment for testicular cancer, your care team may ask if you want to join a research study.
These clinical trials explore new ways to treat the cancer. They may be for people who have not started treatment yet, or who have testicular cancer that came back.
We’re also testing new ways to find cancer and monitor it (surveillance) with our micro RNA(miRNA) research program. miRNAs are genetic material made by tumors that can be found in the blood. We’re using new laboratory methods to isolate (separate) certain miRNAs for use as tumor markers. These markers can help us diagnose and treat testicular cancer.
Most people treated for testicular cancer at MSK are eligible to join this diagnostic trial. A diagnostic trial is a clinical trial studying a new way to diagnose and treat cancer.
Support during and after treatment
MSK has many resources for people living with testicular cancer. We offer guidance on male sexual health and options for preserving fertility and building a family. We also support long-term survivorship after your treatment.
We’re available 24 hours a day, 7 days a week




