Edi Brogi says the best time to get a second opinion is soon after breast cancer is diagnosed, before definitive treatment begins.
A breast cancer diagnosis often starts when a change is found during a breast exam or mammogram. That is usually followed by a breast core biopsy, in which a small sample of the breast tissue is taken and given to a pathologist. A pathologist is a doctor who specializes in diagnosing cancer and other diseases by examining tissue samples using a microscope.
People with breast cancer will probably never meet the pathologist who diagnoses their illness.
Nonetheless, pathologists play an indispensible role in treating people with cancer. They determine the type of breast cancer and the extent of the disease and figure out its weaknesses.
To learn more, we spoke with Edi Brogi, Director of Breast Pathology and an attending pathologist at Memorial Sloan Kettering. Dr. Brogi explains what people should know about breast cancer pathology, including when to get a second opinion.
How does breast cancer diagnosis fit into treating cancer?
A pathologist’s diagnosis is the crossroads of breast cancer treatment. We evaluate the breast tissue under a microscope. We are then able to determine whether the findings are benign (not harmful) or malignant (threatening) and whether treatment is needed.
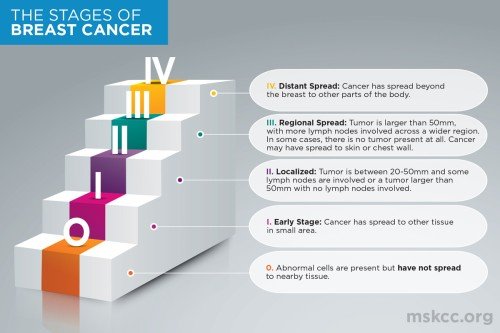
There are many different types of breast cancer, and some are more aggressive than others. A pathologist determines the type of breast cancer and its extent. This includes the size of the cancer and whether it is still confined to the breast or has spread to the axillary lymph nodes or to other parts of the body, such as the bones, liver, lungs, or brain.
All of this information is essential to determining the breast cancer stage. The stage is what doctors use to summarize how advanced a cancer is at the time of diagnosis. At MSK, pathologists are in constant communication with the oncologists and surgeons who treat our patients. I call the pathologist the “doctor behind the curtain.”
How does breast pathology work at MSK?
We see a very large volume of cases, more than 14,000 a year. About 8,000 of those are from biopsies and surgeries performed here at MSK. For these, we review the tissue samples under a microscope and give a diagnosis. With the patient’s permission, we can also run highly advanced molecular tests.
We also perform a large number of second opinions, when we are asked to review a diagnosis given outside our hospital. Because of our expertise, people with cancer, as well as pathologists and doctors at other centers, frequently ask us to review their slides and consult on a diagnosis. Also, when a person comes to us from another hospital, all of the pathology diagnosis done elsewhere is reviewed and confirmed by an MSK pathologist. Second opinions are an integral part of pathology at MSK. We give about 5,000 to 6,000 second opinions a year.
The Breast Pathology team at MSK has nine full-time pathologists devoted exclusively to diagnosing breast diseases. Given the volume and complexity of everything we see, we are all experts in the field. We regularly meet around the microscope to share the most interesting or challenging things we are working on and consult with one another. This gives our team deep expertise, even for the rarest cancers. And it means we can provide a timely diagnosis.
How often do you give a second opinion that substantially changes a diagnosis?
In most instances, a second opinion will confirm the original diagnosis, with only minor changes of no substantial impact for that person.
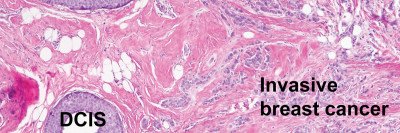
But about 1 to 10% of the time, a second opinion can translate into a substantial change in treatment. For example, take a woman who has been diagnosed with the noninvasive breast cancer ductal carcinoma in situ (DCIS). Sometimes when we’re asked for a second opinion on DCIS, we find microscopic evidence of a small invasive cancer. That finding may require a more aggressive approach, such as a biopsy of the axillary lymph nodes to make sure the cancer hasn’t spread from the breast.
Occasionally the diagnosis will dramatically change the other way. For example, recently I was asked for a second opinion for someone who had been diagnosed with DCIS. When I did my review, I found that no DCIS was present, but instead there was lobular carcinoma in situ (LCIS).
That is great news for the patient because, despite its name, LCIS is not regarded or treated as a real breast cancer. The person did not need to have radiotherapy, which is part of the standard treatment of DCIS but can have major side effects. The patient initiated this request for a second opinion. People often have an instinct to ask for a second opinion and that sometimes can be a very healthy impulse.
When should people get a second opinion? Should they worry that it could delay treatment?
If someone receives a diagnosis of breast cancer and wants to ask for a second opinion, the sooner the better. Certainly a second opinion should be obtained before any definitive surgery, like a mastectomy, or a treatment with substantial side effects, such as radiation therapy or chemotherapy.
People should not worry too much that a second opinion on their breast pathology will delay treatment. A second opinion usually takes a few days or a week. A difficult case may take longer, but that probably really needs a second opinion. In the big scheme of things, that kind of delay has no substantial impact in terms of outcome. It is more important to have the right diagnosis so that the right treatment is given rather than being treated quickly. Think quality over speed.
What should people know about getting a second opinion from MSK for a breast cancer diagnosis?
People can call our consultation office, which can tell them what materials and papers they need to submit. Most insurers will cover a second opinion, although people should always check first. Anyone requesting a second opinion needs to tell us the name and contact information of the doctor to be notified. We give our second opinion to that doctor because doctor-to-doctor communication helps ensure that the appropriate treatment is pursued. If a woman has questions about her diagnosis, she can speak with her doctor, but she can also reach out to the pathologist.
Should all people diagnosed with breast cancer consider getting a second opinion?
Because the diagnosis determines the treatment, or whether treatment is necessary at all, in my opinion it is absolutely critical that the diagnosis is correct. A second opinion provides more certainty. If I were a patient, I would want that.
What new developments in breast cancer pathology should people know about?
Many people are familiar with drugs like tamoxifen (Nolvadex®, Soltamox®) and aromatase inhibitors. These are effective in treating breast cancers with specific hormone receptors.
We are currently learning more about another hormone receptor, the androgen receptor (AR). Androgen is actually a male hormone, but the AR is expressed in many breast cancers. This finding is particularly significant for people with triple-negative breast cancer. This aggressive breast cancer does not respond to treatments targeting the other hormones often found in breast cancer cells.
In clinical trials, some people with metastatic triple-negative breast cancer that has come back showed a good response or no disease progression with androgen-targeted treatments, such as enzalutamide (Xtandi®) and bicalutamide (Casodex®). At MSK, we test the expression of the androgen receptor in all triple-negative breast cancer. There is still a lot of research to be done. But there is reason for hope.