Rapid advances in chimeric antigen receptor (CAR) T cell therapy technologies are in development and under investigation in a range of preclinical and clinical research around the globe.
In our paper, published recently in the journal Expert Review of Hematology, we review the main challenges with current CD19-targeted CAR, obstacles to adopting CAR T cell therapy in solid tumors, and various strategies scientists are pursuing to overcome these issues. (1)
This CAR T Update Part 1 provides an overview of antigen escape, T cell persistence, and safety when using CARs in hematologic malignancies within and beyond the setting of B-cell acute lymphoblastic leukemia (B-ALL). We also provide an overview of the range of different strategies under investigation to address these issues.
Refer to CAR T Update Part 2 to learn about how scientists are building on lessons in the setting of hematologic cancers to find ways to achieve efficacy in solid tumor settings. In Part 2, we also discuss issues related to scaling production and financial accessibility.
Scientists at Memorial Sloan Kettering Cancer Center (MSK) pioneered CAR T cell therapy as a treatment for cancer and were the first to demonstrate that CD19 was a robust target. We continue to explore new ways to advance CAR T cells as a treatment for other hematologic cancers, including lymphoma and multiple myeloma, as well as extending their use to solid tumors, including breast cancer, ovarian cancer, lung cancer, and mesothelioma.
The Evolution of CAR T Cell Therapy
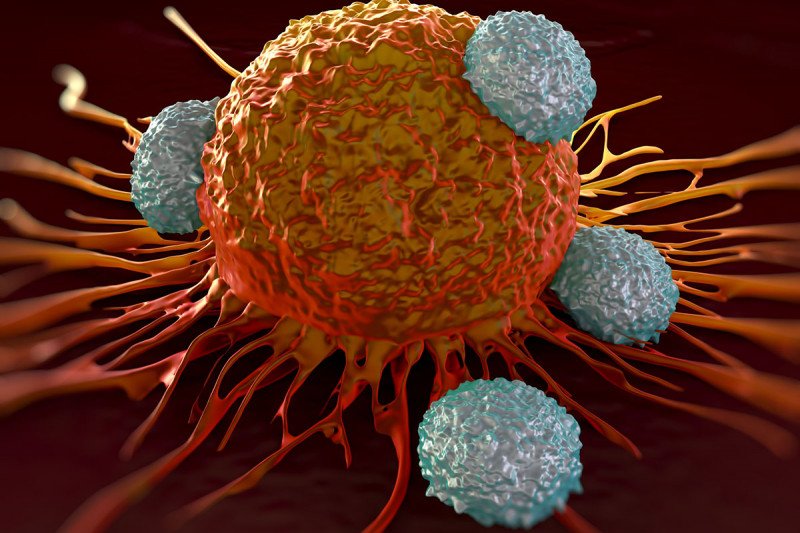
CARs are genetically engineered receptors on T cells. They include a human leukocyte antigen-independent antigen recognition domain, usually in the form of a single chain variable fragment (scFv) from an antibody, combined with a T cell activation domain. (2) Once activated, CAR T cells become cytotoxic against the target antigen.
First-, second-, and third-generation CAR receptors have none, one, or two costimulatory domains, respectively. Newer generations, known as armored CARs, also deliver cytokines or PD1-blocking scFvs, which enhance anti-cancer activity.
Despite the high response rates of 80 to 90 percent achieved with CD19-targeted second-generation CAR T cells in treating B-ALL, (3), (4), (5), (6), (7), (8) they have not had comparable responses in other CD19-positive hematologic cancers, or solid tumors.
Antigen Escape
An epitope is the specific segment of a protein that an antibody binds to. There is evidence of the target epitope loss in B-ALL patients who lose durability of remission after treatment with CD19-directed CARs. (9) Other research suggests that epitope loss may be secondary to deletions, mutations, and alternative splicing of the CD19 antigen recognition domain, allowing tumor cells to escape recognition. (10)
CD19 epitope loss has also led to the emergence of a myeloid clone after treatment for mixed- lineage leukemia (MLL)-rearranged B-ALL in disease recurrence. (11) Interestingly, antigen loss has also been observed in lymphoma (12) and chronic lymphocytic leukemia (CLL) (13) with CAR T cell therapy.
Preclinical models have shown that a process called trogocytosis may play a role in antigen escape with both CD28- and 4-1BB-based CARS. Trogocytosis is an active process that tumors use to transfer the target antigen onto T cells so they can escape destruction. It is believed to be reversible but has yet to be demonstrated in humans. (14)
One solution to overcome antigen escape is to combine single-target CARs that address different targets as a pooled product or use dual CARs (15), (16), (17) or tandem CARs. (18) These combination approaches are currently being tested in clinical trials NCT03330691, NCT03241940, and NCT04029038.
Another approach under investigation is low-dose radiation to sensitize antigen-negative tumor cells to CAR T cells and induce their death through the tumor necrosis factor-related apoptosis-inducing ligand (TRAIL). (19)
T cell Persistence
So far, there is no consensus on the optimal duration of persistence for maintaining long-term remission with CAR T cell therapy. Comparable response rates have been observed with a median duration of persistence of 14 days (3)and 168 days. (4)Still, relapses have been observed in some cases where CARs were no longer performing immunosurveillance. (8)
T-cell stimulation is a double-edged sword: It increases persistence, but overstimulation can result in exhaustion. (20) Some researchers have demonstrated that longevity can be improved without compromising efficacy by eliminating a signaling redundancy, or by placing immunoreceptor tyrosine-based activation motifs (ITAMS) near the membrane. (21)
A well-studied explanation for decreased persistence of CAR T cells is transgenic immune responses against scFv of murine origin. (22), (23), (24) A fully human scFv-based CAR has shown promising activity against the target antigen in preclinical research. (25) It may be possible to use human scFv-based CARs as a salvage therapy against the same antigen in patients treated with murine-scFv CARs, as shown in a study among B-ALL patients. (26) Clinical trials using humanized (NCT02374333), as well as fully human scFv-based CARs (NCT03684889 and NCT03602612), are in progress.
Several groups have studied central memory (27), (28) and stem cell memory T cells (29), (30), (31), (32) to learn more about persistence mechanisms in adoptive cell therapy (example: CARs). Approaches using defined ratios of CD4:CD8 T cells revealed that the CD4 subset is vital for boosting overall anti-tumor activity. (33), (34) Ongoing clinical trials in this area are NCT01318317, NCT01815749, NCT03389230, and NCT02706405.
Persistence and reduced exhaustion in CAR T cells have been achieved by optimizing the ratio of CD4:CD8 cells through alterations to signaling domains and pathways. (35) Another promising design modification involved diminishing redundant signaling, which improved effector/memory cell ratios and CAR persistence. (21)
An alternative approach to improve persistence involves stimulating the T-cell receptor using antigens from viruses, such as the Epstein-Barr virus (EBV) or cytomegalovirus (CMV), and then using the cytotoxic T cells to transduce CARs. Clinical trials underway testing this approach with hematologic and solid tumor antigen-directed CARs are NCT00085930, NCT01109095, NCT03768310, NCT01460901, and NCT01953900.
Finally, tumor vaccines and antigen presenting cells (APCs) may provide an immunological boost to CAR efficacy and persistence. See NCT01953900, NCT02482532, and NCT03186118.
Safety
One of the biggest challenges with CAR T cell therapy is the potential for toxicity, since healthy cells may express the same targets as cancer cells. Cell engineers are incorporating “off” and “on” switches and employing other strategies to mitigate toxicity.
CARs with “off” switches, also called “suicide genes,” can be rapidly destroyed when toxicities arise or after they have eliminated cancer cells. (36), (37), (38), (39) Dasatinib has recently shown it can pause CAR T cell activity temporarily, acting as a reversible switch. (40) Current trials investigating safety “off” switches include NCT02414269, NCT03696784, NCT03500991, NCT02311621, and NCT03016377. Other strategies for inactivating CARs involve checkpoint blockade, (41) titrating activation with an antibody switch, (42) and using self-limiting or transient CARs. (43), (44), (45), (46)
“On” switches activate CARs only in the presence of an activating entity. (47) A platform called GoCAR-T, where a small molecule activates the costimulatory signal only when target antigen- CAR interaction is present, is currently being tested in clinical trials. Recent data from NCT02744287 showed the approach effectively boosted expansion and persistence in four patients. (48) The safety of the GoCAR-T platform may be further strengthened by adding an “off” switch. (49) Another approach is to use synthetic NOTCH receptors that sense environmental cues and function as “smart” CARs. (50)
Toxicities associated with CAR T cell therapy are cytokine release syndrome (CRS) and neurotoxicity, including temporary headache, confusion, and delirium. High-grade CRS, an acute inflammatory response characterized by fever and multiple organ failure and fever, is rare but can occur.
Beyond safety switches, scientists are investigating ways to reduce toxicities without compromising efficacy. For example, one strategy is the prophylactic administration of tocilizumab, an interleukin-6 (IL-6) blocking antibody (see NCT02906371), or an IL-1 antagonist. (51)
Emerging evidence in the setting of CD19-directed CARs for B-ALL shows that the severity of CRS depends on tumor burden. (7), (8), (52) Therefore, strategies to reduce the risk of CRS include optimizing patient selection, changing the conditioning regimen, (53) and using a split-dose approach (54) for CAR T cell infusion.
Advancing CAR T Innovation
At MSK, we are dedicated to finding new ways to improve patient outcomes through groundbreaking preclinical and clinical research. We are currently conducting 15 clinical trials testing CAR T cell therapy in a range of indications, including lymphomas, multiple myeloma, advanced breast cancer, mesothelioma, and lung cancer.
The paper was not funded. Dr. Namuduri is an adhoc consultant for Cellectar Biosciences. Dr. Brentjens receives royalties and grant support from JUNO Therapeutics and is a consultant for JUNO/Celgene. The authors have no other relevant affiliations or financial involvement with any organization or entity with a financial interest in or financial conflict with the subject matter or materials discussed in the manuscript apart from those disclosed.