The largest retrospective study ever done to assess the impact of hepatic arterial infusion (HAI) chemotherapy on survival outcomes in people with colorectal cancer with liver metastases has shown that the addition of HAI extends survival by almost two years.
The results of the study, conducted at Memorial Sloan Kettering (MSK) over a 21-year period and published in June 2017 in the Journal of Clinical Oncology, are remarkable considering that those in the HAI group had more-advanced disease before treatment. (1)
Colorectal cancer is the third most common cancer in the United States, with an annual incidence of 137,000 people, (2) and it is a major cause of death. (3) In patients with metastatic disease over half of the patients will develop liver metastases, a leading cause of mortality. For patients who undergo tumor resection, the overall survival rate at ten years is typically about 20 percent for patient receiving systemic alone after resection. (4)
Unfortunately, after resection, most people develop recurrent disease,4 and the liver is the only site of first recurrence for about half of all people. (5) Systemic chemotherapy has traditionally been the standard of care to delay or prevent disease recurrence. However, randomized controlled trials have not demonstrated a significant difference in overall survival compared with those who did not receive systemic chemotherapy. (6), (7)
For more than 30 years, medical and surgical oncologists at MSK have been pioneering liver-directed HAI chemotherapy, a treatment approach that is demonstrating significantly improved survival rates for people with colorectal cancer with resectable colorectal liver metastases. MSK is one of a few centers in the United States using the technique, and we recently shared our expertise with medical and surgical oncologists visiting from several institutions around the country and Europe to learn from our team.
HAI Provides a Significant Survival Advantage
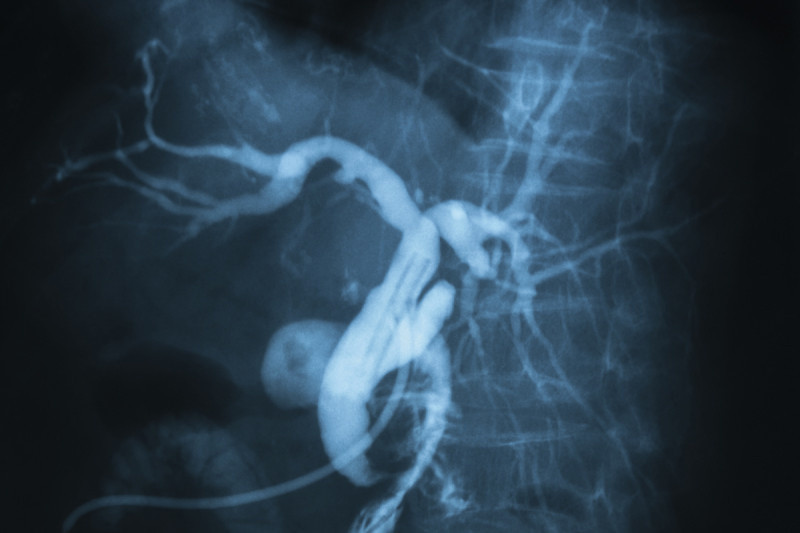
HAI involves surgically implanting a pump about the size of a hockey puck under the skin between the ribs and pelvis. This occurs during the same surgery as the tumor resection. The pump delivers chemotherapy to the liver through the hepatic artery, which supplies most of the blood to colorectal liver metastases. The agents deployed have a high first-pass extraction in the liver, allowing the use of high doses with limited systemic impact.
From 1992 to 2012, we evaluated 2,368 people who had complete tumor resection and compared survival rates for the group that received perioperative HAI with the group that did not. All of them also received standard systemic chemotherapy. (1)
For the HAI group (n=785), median overall survival was 67 months compared with 44 months for the non-HAI group (n=1,583, p < .001). Five-year overall survival was 53 percent for the HAI group compared with 38 percent for the group that did not receive a pump (p < .001), and ten-year survival rates were 38 percent and 23 percent (p < .001), respectively. (1)
We also examined data for the most recent cohort of 1,442 people to see if our findings would hold, given that during the 21-year period, more-modern systemic chemotherapy agents became available. The results were similar: The median overall survival was 67 months with HAI and 47 months without (p < .001). (1)
Additionally, we identified who was most likely to benefit from HAI — those with node-negative colorectal cancer (129 months survival with HAI chemotherapy compared with 51 months without, p < .001) and a low clinical risk score (89 months with HAI compared with 53 months without, p < .001). (1)
Achieving Higher Survival Rates
In our recently published study of MSK patients with metastatic colorectal cancer who received liver tumor resection, HAI, and systemic chemotherapy, we examined survival outcomes for those treated before and after 2003. The group treated after 2003 experienced significantly higher five- and ten-year survival rates, 78 percent and 61 percent, respectively, compared with 56 percent and 40 percent, respectively, for the group treated before 2003. (8)
The higher survival rates for the most recent group reflect the development of new systemic chemotherapy agents, such as irinotecan and oxaliplatin molecular targeted agents, such as vascular endothelial growth factor inhibitors and epidermal growth factor inhibitors; and improvements in surgical techniques. At the time of publication, median overall survival had not been reached for the group treated after 2003. (8)
Given the greatly improved survival outcomes possible today, we recommend that people with resectable disease undergo resection and see a multidisciplinary team of cancer care experts to consider HAI chemotherapy. It is a complex treatment protocol that requires skill and experience: Surgical pump placement after resection requires learning about 25 procedures; avoiding biliary toxicity requires intensive management by a medical oncologist; and nuclear medicine specialists, interventional radiologists, and gastroenterologists should also be involved to manage potential complications, such as bleeding or ulcer disease.
At MSK, we are conducting clinical trials to look for new ways to improve survival outcomes for our patients, including those with unresectable tumors. For example, we have a phase II trial underway to evaluate the use of HAI and intravenous chemotherapy compared with intravenous chemotherapy alone in people with inoperable colorectal liver metastases.