MSK is the first hospital in New York City to offer gene therapy through its pediatric cancer program MSK Kids. Exagamglogene autotemcel (exa-cel) (Casgevy®) is a gene therapy for treating sickle cell disease in patients 12 years and older with recurrent vaso-occlusive crises and transfustion-dependent beta thalassemia in the same age group.
“MSK has a long track record of treating patients with sickle cell disease and thalassemia, including providing curative bone marrow transplantion,” said Andrew Kung, MD, PhD, Chair of the Department of Pediatrics and the Lila Acheson Wallace Chair for Pediatric Research at MSK. “Following our leadership in gene therapy clinical trials, this authorization expands our treatment options for these underserved patient populations.”
In this Q&A with Jaap-Jan Boelens, MD, PhD, Chief of the Pediatric Transplant and Cellular Therapy Service at MSK, we discuss MSK Kids’ authorization, the new gene therapy and how it works, its benefits and risks, and MSK’s dedication to advancing treatment options for pediatric and young adult patients with hemoglobinopathies.
When did Vertex Pharmaceuticals authorize MSK Kids to provide the first gene therapy for sickle cell disease and beta thalassemia?
The U.S. Food and Drug Administration approved exa-cel in December 2023. (1) After careful vetting as a center of excellence in providing cellular therapies, Vertex approved MSK Kids as an Authorized Treatment Center for exa-cel in early November 2024.
How does the gene therapy work?
Sickle cell disease is an autosomal recessive disorder caused by mutations in the hemoglobin β gene (HBB), which encodes adult hemoglobin. The most common mutation replaces glutamic acid with valine at amino acid position 6, resulting in sickle-shaped red blood cells that cause painful vaso-occlusive episodes, anemia, organ damage, and a reduced lifespan. Disease symptoms appear after birth as γ-globin gene transcription of HGB1 and HGB2 changes to HBB, causing a shift from fetal hemoglobin to adult hemoglobin in red blood cells. (2)
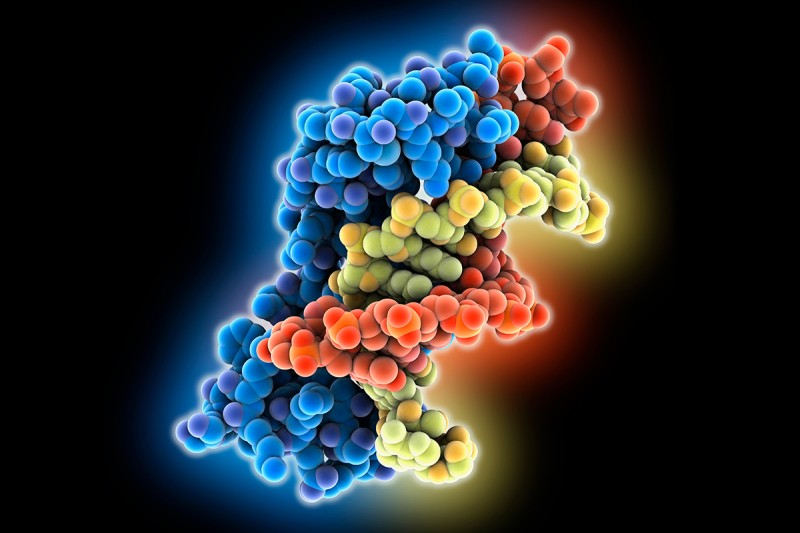
Exa-cel is a one-time therapy made by editing a patient’s own hematopoietic stem cells using CRISPR/Cas9 technology. The transcription factor BCL11A is edited so that it no longer suppresses the production of fetal hemoglobin in red blood cells. (3) After the stem cells are infused back into the patient, they promote the production of fetal hemoglobin, which prevents sickling. For patients with beta thalassemia, the increase in fetal hemoglobin addresses the insufficient quantity and function of adult hemoglobin.
What is the timeframe from identifying an eligible candidate to gene therapy infusion?
The time frame is about seven months from an agreement for coverage to infusion.
What does treatment with exa-cel involve for patients?
Patients are taken off hydroxyurea, the standard-of-care disease-mitigating chemotherapy for increasing fetal hemoglobin, to allow their bone marrow to recover and put on red cell exchange transfusions. That takes about two months.
Next, we mobilize their stem cells with plerixafor, and two hours later they go to the apheresis room for stem cell collection. Note that we can’t use granulocyte-colony stimulating factor as we do for patients with beta thalassemia because that would significantly increase the risk of pain crises in patients with sickle cell disease.
Collecting a sufficient quantity of stem cells for the cell product may take more than one apheresis cycle, which is two days of collection. In the clinical trial, the median number of cell collections cycles was two (one-third of patients required one, one-third needed two, and one-third required more than two sessions). The cells are sent to the manufacturer’s facility and we get them back 16 to 20 weeks later after they have been gene-edited.
Patients are admitted for myeloablative conditioning with busulfan before receiving an infusion of the gene modified product. Engraftment takes about three to four weeks after stem cell infusion, followed by four or five weeks for platelet recovery.
What are the main benefits of treatment with exa-cel and what are the risks?
Exa-cel provides a potential cure for sickle cell disease in a one-time treatment. The phase 3 clinical trial that led to its approval (NCT03745287) found that exa-cel eliminated vaso-occlusive crises in 97% of patients ages 12 to 35 for 12 months or more. The percentage of red cells expressing fetal hemoglobin was 70% at three months and greater than 93% after six months. (4)
This gene therapy eliminates the need for allogeneic bone marrow transplantation (allo BMT). While allo BMT is a curative treatment option, it is extremely challenging to find suitably-matched donors and the procedure carries a risk of graft-versus-host disease (GVHD) and a 10% mortality risk. As exa-cel is an autologous cell therapy, there is zero risk of GVHD.
In the clinical trial, the safety profile of exa-cel was consistent with what we typically see with busulfan myeloablative conditioning in allo BMT. Severe adverse reactions occured in 45% of patients after conditioning and exa-cel treatment, such as cholethithiasis, pneumonia, and pain, which is the reason the treatment is restricted to centers of excellence with the expertise to manage expected treatment effects. (5)
The longest follow-up in the clinical trials was about four years, so the long-term benefits and risks associated with exa-cel are not yet known. For some patients, particularly older people who were treated with hydroxyurea for decades, there is a small increased risk of developing myelodysplastic syndrome (MDS) or acute myeloid leukemia (AML). Among hundreds of patients treated, there will be an occasional patient that develops MDS or AML, but it’s important to recognize that patients with sickle cell disease have a baseline increased risk compared to those without the disease.
How does treatment with exa-cel compare to other treatment options for patients with sickle cell disease?
Standard treatment options such as hydroxyurea help mitigate the severity of vaso-occlusive crises and pain events, but do not address the central cause of the disease and cannot provide curative potential. The induction of fetal hemoglobulin with hydroxyurea is much lower than with exa-cel.
Keep in mind that allogeneic bone marrow transplantation (allo BMT) is a proven curative therapy, whereas the long-term benefit of exa-cel unknown. We consider each patient’s case carefully and present them with personalized options.
Exa-cel is approved for patients 12 and older and was tested in the clinical trial among patients ages 12 to 35. Does MSK offer this therapy to patients over 35?
If there is a suitable patient over 35, we would consider treating them with exa-cel. We also have a track record of expertise treating adults with sickle cell disease with allo BMT. In fact, some of our older sickle cell patients are willing to take on a 10% mortality risk with allo BMT because they are so fed up with the disease and know that things will only get worse with age.
That being said, older patients who have accumlulated a lot of antibodies from years of red blood cell transfusions are not good candidates for exa-cel because they would require a significant number of red cell exchanges — more than we have available through our transfusion medicine group. These patients would be better candidates for allo BMT. They would still require red cell infusions, but to a lesser extent that is more manageable by the blood bank.
Did MSK Kids participate in the clinical trials of gene therapy for sickle cell disease?
Yes, and from that experience, we learned a lot about managing patients throughout the treatment process, from preparation and mobilization to infusion and post-treatment care. Our multidisciplinary team includes the transfusion medicine group, transplant specialists, and pain specialists, who are dedicated to providing excellent care throughout the gene therapy treatment process.
The one-time treatment cost of exa-cel is about $2.2 million. Does Medicaid cover the cost?
New York State Medicaid has not yet officially released its coverage policy for exa-cel. However, they are considering requests for coverage on a case-by-case basis.
For example, I submitted a letter of medical necessity for our first patient, and Medicaid approved it overnight. The patient is an 14-year-old male who experienced 12 events over the past two years, including eight hospital admissions for vaso-occlusive crises and four urgent care visits for intravenous pain medication. Eligibility for exa-cel is at least four events in two years.
We continue to submit requests on a case-by-case basis, and decisions are typically taking about four to six weeks. In fact, Medicaid has asked us to continue to request coverage for medically appropriate cases because that will help them formulate an approved product listing. I anticipate they will include exa-cel as a covered therapy sometime in the coming year.
What other treatment avenues is MSK exploring for sickle cell disease?
We are currently collaborating with a group in Marseille, France on an allo BMT clinical trial (NCT05736419) using a haploidentical post transplant cyclophosphamide protocol aimed at preventing graft failure and reducing the risk of GVHD in patients with sickle cell disease or beta-thalassemia. The trial is open to pediatric patients, young adults, and adults at MSK’s main campus. In Manhattan. Our goal is to recruit at total of 24 patients at MSK. So far, we have treated five and our colleagues in Marseille have treated five. The median age has been about 28, ranging from 21 to 46 years.