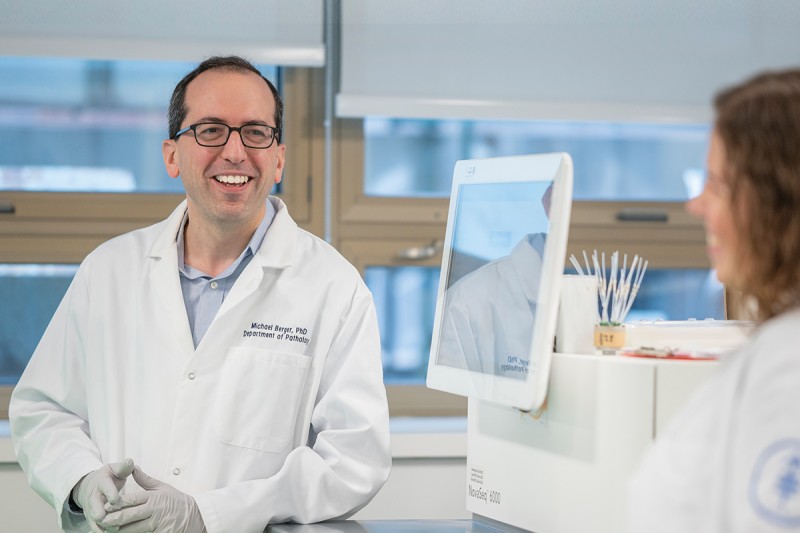
Dr. Michael Berger is focused on developing new methods to characterize the genetic makeup of individual cancers.
It was a major milestone a decade in the making. Inside a bustling lab at Memorial Sloan Kettering Cancer Center (MSK) on an otherwise ordinary Thursday in February 2023, specially trained technicians performed a unique test for the 100,000th time. The test was to analyze DNA from a patient’s tumor sample. This extraordinary tool allowed doctors to diagnose the exact type of cancer with exquisite precision, just as it had done 99,999 times before.
The landmark sample came from an MSK patient in their late 40s with colorectal cancer. The tumor was analyzed with a cancer genetic test called MSK-IMPACT®, which examines tumor tissues to look for cancer-causing mutations (changes) in more than 500 genes. The goal: Target that mutation with a drug.
“The tumor had a total of 50 mutations detected by MSK-IMPACT®, a number that’s about seven times higher than the typical colorectal cancer,” says cancer geneticist Michael Berger, PhD, Co-Director of the Marie-Josée and Henry R. Kravis Center for Molecular Oncology and Elizabeth and Felix Rohatyn Chair for Junior Faculty. “Three of those mutations can be targeted with existing drugs.” But even more hopeful, the test revealed that this patient’s own immune system could potentially be enlisted to fight the cancer cells.
Treating Cancer Based on Its Genetic Mutations — Rather Than Its Location
Researchers have known for several decades that cancer cells contain gene mutations that cause them to grow out of control. Peering deep into the chaos of cancer cells, tumor DNA sequencing tests developed at MSK uncover all kinds of changes in their genes. Also known as molecular tests, they provide important clues to understanding what makes each individual tumor unique — and often reveal weaknesses that can be targeted with an expanding arsenal of treatments.
In 2017, MSK-IMPACT® was the first test of its kind to be authorized for patients by the Food and Drug Administration (FDA). A related test also developed at MSK called MSK-ACCESS® was approved for clinical use in 2019. Known as a liquid biopsy, this test analyzes bits of DNA shed from tumor cells that can be found in a blood sample. It can help monitor whether a patient is responding to treatment.
Dr. David Solit studies how genetic changes in tumors support growth, metastasis, and other aspects of cancer.
Together, the tests developed at MSK have helped revolutionize the way cancer is treated around the world. Therapies are no longer chosen based solely on where a tumor arises in the body. Instead, the tumor’s unique molecular characteristics guide treatment decisions.
“As more and more targeted therapies and immunotherapies become available, it becomes critical to be able to predict which patients are most likely to benefit from each treatment option,” says physician-scientist David Solit, MD, Geoffrey Beene Chair, who studies how patients respond to precision oncology therapies. “The results of tumor and liquid biopsy testing can also tell us which patients may be eligible for clinical trials,” he adds.
Dr. Solit is the Founding Director of the Center for Molecular Oncology, established in 2014 thanks to a generous gift from The Marie-Josée and Henry R. Kravis Foundation.
Special Benefits for MSK Patients
MSK’s cancer DNA tests are offered to thousands of patients every year. The cost is covered by most insurance plans or through the generosity of philanthropic donations.
Unlike tests used at most other hospitals, MSK’s tumor sequencing also includes a sample of a patient’s normal DNA. That’s how doctors can determine whether the cancer-causing mutation is present exclusively in the cancer cells or was inherited from a parent. This knowledge is vital for patients’ families, who may be completely unaware that an increased cancer risk lurks in their genes. In some cases, identifying an inherited cancer mutation also suggests which types of drugs may work.
There’s a mind-boggling amount of data about cancer mutations and potential drugs, so MSK researchers have pioneered another important tool for precision oncology: OncoKB®. OncoKB® is a database that’s accessible nationwide to help doctors match the right drugs to their patients, based on their tumor DNA tests.
Discovering New Cancer Drugs Based on Genetic Mutations
Molecular tumor tests don’t only identify the best treatments available for patients today. They also have changed the approach to researching the best therapies of tomorrow.
“It used to be that you’d organize a clinical trial to recruit patients who all had the same type of cancer,” Dr. Berger says. “But as we’ve gotten better at recognizing which drugs were likely to target which mutations in someone’s tumor, we discovered that people with many different kinds of cancer could benefit from the same drug because they all share mutations in the same gene.”
Unfortunately, MSK’s disease detectives haven’t solved all cases. In about 5% to 10% of patients, the underlying genetic cause of the cancer cannot be found. And in more than half of patients, even when the tests can detect the culpable mutations, no drugs are available yet to target them.
“The field of pharmacology has made huge progress developing effective therapies for certain mutations,” Dr. Solit says. “But there are still dozens of genes that contribute to cancer that do not yet have a drug available for clinical use. They are in development, but more work needs to be done.”
As thousands of tumors continue to be tested at MSK, there will be more milestones ahead, revealing even more ways to crack cancer’s code — and end it for life.
Thanks to MSK Tests, Rick Avoided Surgery

This time, hoping for an effective drug treatment instead, Rick came to MSK. The MSK-IMPACT® test revealed his tumor, called a liposarcoma, was caused by a mutation in the gene MDM2. He got encouraging news from his doctors, sarcoma experts Samuel Singer, MD, and Mrinal Gounder, MD, who said he could participate in an early-stage clinical trial (research study) of a drug targeting that mutation.
“I was so grateful when I learned I could enroll in a clinical trial rather than have surgery,” Rick says.
More than a year later, the tumor has stopped growing. Rick, now 64, remains on the drug and is managing the side effects that have reduced his appetite and his energy. Now retired from his job as head of the Brooklyn Hispanic Chamber of Commerce, Rick is still an active member of the business community. He helps to run the NYC Racial Justice Reporter, a digital and print media outlet that promotes women- and minority-owned businesses in New York City.
“The nurses at MSK are the highest quality and very compassionate,” Rick says. “I’ve got the best doctors in the world. I feel so confident in my care.”
MSK Test Reveals a Family’s Risk
Three generations of the Deutsch family are under the watchful eye of MSK experts, after Judah Deutsch was treated for a benign brain tumor when he was 7.

Three generations of the Deutsch family — (from left) Lenny, Judah, and Michael — are being followed by doctors at MSK after genetic testing revealed a hereditary cancer gene in their family.
MSK-IMPACT® testing revealed that he had a rare mutation in the SDHD gene. It did not cause his brain tumor, but it is linked to other tumors. Michael Walsh, MD, a pediatric oncologist and geneticist at MSK Kids, recommended testing to learn if others in the family were at risk. It turned out Judah’s father, his grandfather, and one of his brothers all had the mutated SDHD gene.
In the eight years since Judah was first treated, both he and his dad, Michael, developed benign growths in their neck arteries, called paragangliomas, which are related to SDHD. Caught early, Michael’s first tumor was surgically removed and a second one is being monitored. Judah’s paraganglioma was treated successfully with proton radiation therapy.
Many years ago, Judah’s grandfather Lenny had been treated for a different tumor — a rare stomach cancer called GIST (gastrointestinal stromal tumor), which is also linked to the SDHD mutation. He is now being monitored for additional tumors linked to this gene.
“Our whole family sees Dr. Walsh,” Michael says. Everyone with the mutation is scanned regularly at MSK. And, happily, all are doing well.
“The Deutsch family’s story goes beyond using genetic testing for people with cancer,” Dr. Walsh says. “It illustrates our opportunity to improve the lives of families for generations. They’ll know to be screened so any tumors can be caught and managed early.”