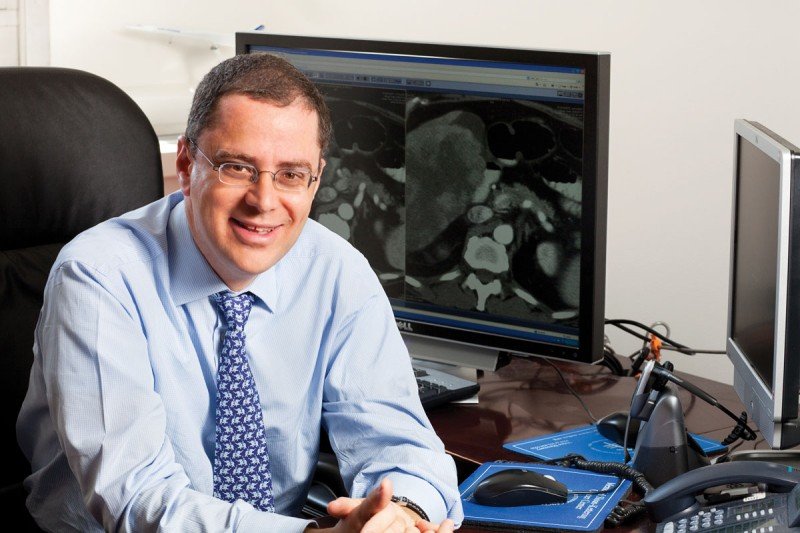
New research from Memorial Sloan Kettering Cancer Center (MSK) led by medical oncologist Ghassan Abou-Alfa, MD, and colleagues, found that a combination of the immunotherapy drugs durvalumab (IMFINZI®) plus the experimental drug tremelimumab significantly improved overall survival in people with unresectable hepatocellular cancer, compared with people who received sorafenib (NEXAVAR®), a current standard of care. Dr. Abou-Alfa will present the results from the randomized phase 3 HIMALAYA trial at the press program of the American Society of Clinical Oncology (ASCO) Gastrointestinal Cancers Symposium, taking place January 20–22, 2022, in San Francisco.
In this phase 3 randomized HIMALAYA trial, Dr. Abou-Alfa and a team of investigators evaluated 1,171 patients with unresectable hepatocellular carcinoma (liver cancer). In the study, people were randomized to one of the three following treatment regimens: STRIDE (Single Tremelimumab Regular Interval Durvalumab), the immunotherapy combination that was given intravenously every four weeks; durvalumab alone; and sorafenib. Dr. Abou-Alfa and colleagues theorized that a single dose of tremelimumab would improve the response to durvalumab.
The combination immunotherapy was based on the notion that adding checkpoint blockade against CTLA-4 (tremelimumab) to treatment with checkpoint blockade against PD-1 (durvalumab) would be more effective than treatment with a PD-1 drug alone. The tremelimumab was given only once at the beginning of treatment to jump-start the immune response.
Researchers followed trial participants’ health for a median of about 33 months from when they received their first treatment in the trial. At that time, the overall response rate for patients who received the combination treatment was 20.1%, compared with 17% for those who received durvalumab alone and 5.1% for those who received sorafenib. Patients who received the combination had a 22% lower risk of dying, compared with those who received sorafenib. Serious (grade 3 or 4) side effects were worse for the combination than for durvalumab alone (25.8% versus 12.9%), but they were still better than the side effects for sorafenib (36.9%).
“We are very encouraged by the data and the results of the study,” said Dr. Abou-Alfa. “Despite available therapies for unresectable hepatocellular cancer, new options are needed to improve long-term disease control and patient survival. These findings have the potential to change the standard of care for liver cancer. Pending a potential FDA approval, this novel dual immunotherapy regimen could be readily available to all patients and would not require any additional safety assessments prior to treatment.”
This international trial was conducted in the United States, Canada, and 14 other countries, including those in Europe, South America, and Asia.
In January 2020, the U.S. Food and Drug Administration granted durvalumab plus tremelimumab orphan drug status for hepatocellular carcinoma. An orphan drug designation is given to drugs that are intended for the treatment, diagnosis, or prevention of rare diseases or disorders that affect fewer than 200,000 people in the United States.
Making New Advances for Liver Cancer Patients
Cancer immunotherapy was born at MSK a little more than a century ago. Since then, physician-scientists across MSK have led the effort to develop immune-based treatments for different types of cancer. MSK has been at the epicenter of discoveries in the field, and the institution’s work is bringing exciting new treatment options to people around the world. MSK physicians have extensive experience using immunotherapy to treat people with melanoma, kidney cancer, lung cancer, bladder cancer, and other cancers, as well as handling immune-related side effects.
The National Cancer Institute estimates there were about 42,230 adults diagnosed with primary liver cancer in the United States in 2021, with an estimated 30,230 deaths due to the disease. The overall liver cancer death rate has doubled since 1980. The most recent five-year survival rates are 32.6% in people diagnosed with localized liver cancer, 10.8% with regional disease, and 2.4% with distant disease.
“As physicians, we consistently strive to provide our patients with the most effective therapies and give those with advanced disease more options,” said Dr. Abou-Alfa.
This trial was sponsored by AstraZeneca.
