The ability to identify an individual’s specific tumor type prior to surgery could have important implications for the management of patients diagnosed with kidney cancer. A newly published study demonstrates that imaging with Positron Emission Tomography (PET) using a radiolabeled antibody accurately identifies whether a patient has clear cell renal carcinoma - the most common and aggressive type of renal tumor - and arms the urologist with crucial information that will help determine whether surgery is needed.
Conducted by researchers at Memorial Sloan Kettering Cancer Center (MSKCC), the study will be published in the April 2007 issue of The Lancet Oncology and available online March 6.
“This work represents the first prospective clinical trial to determine whether PET using a radiolabeled antibody is sensitive and specific enough to permit identification of clear cell renal carcinoma,” said the study’s lead author, Chaitanya Divgi, MD, who is now Chief of Nuclear Medicine and Clinical Molecular Imaging at the University of Pennsylvania.
In the study, the researchers used the radiolabeled monoclonal antibody G250, which was originally developed as a potential therapeutic agent by study co-author Lloyd J. Old, MD, Director of the New York Branch of the Ludwig Institute for Cancer Research (LICR), and an investigator at MSKCC. G250 has since been shown to target and bind to clear cell renal carcinoma and to react against an enzyme that is present in 94 percent of these cancers. Studies have also demonstrated that renal carcinoma has the highest recorded tumor uptake for G250 of any solid tumor, making the antibody ideal for use with PET imaging for this disease.
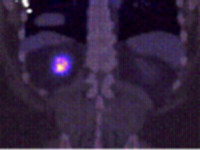
PET is a highly specialized, noninvasive imaging technique that uses short-lived radioactive substances to produce three-dimensional color images of those substances functioning within the body. Unlike CT (computerized tomography) and MRI (magnetic resonance imaging), which provide anatomic images, PET scanning provides information about the body’s chemistry, metabolic activity, and body function not available through other procedures.
According to the study, 15 out of 16 clear cell renal carcinomas were correctly identified using G250 PET, resulting in a sensitivity of 94 percent. All 9 patients with non-clear cell renal masses were negative on the PET scan - which is highly predictive of a less aggressive cancer - resulting in a specificity of 100 percent.
“Antibody PET could end up changing the standard of care for patients with kidney cancer,” said the study’s senior author, Paul Russo, MD, a urologic cancer surgeon at MSKCC. “The excellent sensitivity and specificity of this tool supports the utility of G250 PET imaging in the work-up and management strategies for clinically localized renal masses and as an alternative to biopsy for distinguishing renal lesions.”
In the study, 25 patients scheduled to have surgery to remove a renal mass received intravenous 124I-cG250. PET images obtained prior to surgery were graded as positive or negative for antibody uptake. A pathologist unaware of PET scan results then classified resected tumor specimens as clear cell renal carcinoma or otherwise.
All patients were monitored for toxicity and the antibody infusion was well tolerated with no side effects or other adverse events related to the agent.
According to the authors, G250 PET may ultimately be used not only to determine the aggressiveness and extent of a patient’s disease prior to any surgical intervention, but also to measure the therapeutic effects of a particular treatment, and predict the likelihood of recurrence.
“The promising results of this trial have stimulated interest in a larger, prospective multi-center trial to confirm our findings, and ultimately greatly improve the clinical management of patients with kidney tumors,” said Dr. Divgi.
There were an estimated 38,890 new cases of renal carcinoma in the United States in 2006, and an estimated 12,840 deaths due to the disease. The majority of cases of renal tumors are confined to the kidney and 30 percent of patients either present with, or later develop, metastatic disease. Of those patients who either present with or later develop metastatic renal cancer, approximately 90 percent of these tumors have the most common clear cell histological subtype when examined under a microscope.
