
Just after a cancer diagnosis, perhaps the last thing on your mind is how treatment might affect how or what you eat. But cancer itself — along with side effects from treatments such as chemotherapy, radiation, and surgery — can significantly impact your appetite, eating habits, activity levels, and weight.
Most cancer patients lose weight during treatment, though certain therapies — particularly those for hormone-driven malignancies such as breast and prostate cancers — can trigger weight gain. Getting back to a “normal” diet after treatment is completed poses its own challenges. Since significant weight loss or gain can affect your prognosis (chance of recovery), careful weight management should not be an afterthought.
Here, Memorial Sloan Kettering registered dietitian/nutritionists Christina Stella and Suzanne Gerdes share tips on how to best manage weight and diet during and after cancer treatment.
Don’t restrict yourself to certain foods.
Chemotherapy and radiation treatments can cause a host of side effects that make it difficult or unpleasant to eat, including nausea, taste changes, and mouth sores, among other things. But many patients, as soon as they receive a cancer diagnosis, decide to restrict their diets in hopes of offsetting years of bad eating habits, Ms. Stella explains.
“All of a sudden they’re going vegetarian, saying they’ll never eat sugar again, or everything has to be organic,” she says. “But they don’t know how chemo or radiation will affect them, and then they start struggling. It’s not a good idea to restrict your diet when treatment already cuts down on what you’ll want or be able to eat.”
“Research suggests that eating a variety of foods is better for your health,” Ms. Gerdes adds. “Unless your doctor advises you to avoid specific foods for medical reasons, you should not restrict certain foods or nutrients, since they may not change the course of your cancer.”
On some days, it’s enough to just eat.
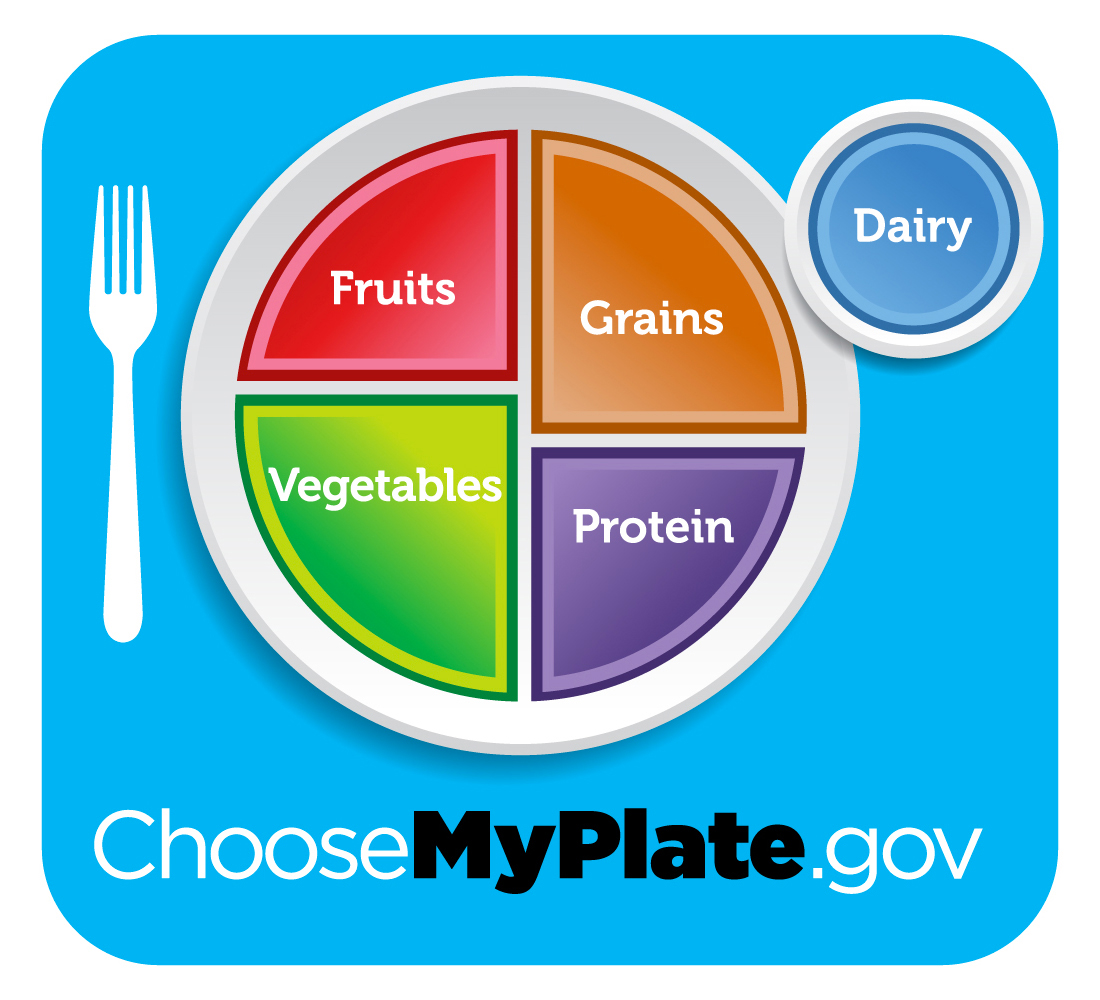
Ideally, Ms. Stella explains, patients currently undergoing treatment will use a modified version of the USDA’s MyPlate icon to guide their nutritional intake. But instead of splitting the plate down the middle — with protein and carbohydrates occupying one side and fruits and vegetables on the other — these patients should aim for a “peace sign” consisting of equal portions of fruits and vegetables, carbohydrates, and lean protein. It’s beneficial for cancer patients to increase the amount of protein they eat, since adequate protein intake is particularly important to avoid losing lean muscle mass when dropping weight.
This goal changes, however, when patients don’t feel well enough to eat much of anything.
“For those having difficulty maintaining their weight, it can get to the point where any calorie is really more important than being picky about food choice,” Ms. Stella says. “Too much concern about types of food can give the patient a lot of anxiety. Just eat.”
Stay hydrated.
Staying hydrated is important for all cancer patients to help their bodies deal with the effects of treatment. But for those trying to stem weight loss, it’s also an opportunity to add calories to their diet in a taste-friendly way.
“If our goal is to add calories when hydration becomes more important, then why not combine both?” Ms. Stella asks.
“Water and drinks with calories, like 100 percent fruit juice, do the same thing,” Ms. Gerdes adds. “They keep you hydrated.”
Keep as active as possible.
Fatigue is such a prevalent side effect of many cancer treatments that patients may find it difficult to get off the couch on some days, much less head outside for a walk. But staying physically active is important for weight management regardless of whether weight loss or gain is desired because regular movement helps maintain lean muscle mass.
“We really want patients to hold on to their muscle mass because research has told us there are poorer prognoses for patients who lose their lean body mass at a very rapid rate,” Ms. Stella says.
If you’re looking for a class, take a look at the fitness and yoga classes on offer at MSK’s Bendheim Integrative Medicine Center. Anyone can join.
Put the brakes on supplement use.
Eating whole foods, and getting the nutrients your body needs from them, is the gold standard of nutrition. In fact, vitamins and other supplements — which aren’t regulated by the US Food and Drug Administration or any agency — can actually interfere with certain cancer treatments and medications.
“It depends on what treatment you’re on and what supplement you’re taking,” Ms. Gerdes says, “but supplements are definitely something we want our patients to avoid most of the time because they’re taking so many medications, we don’t know what’s going to interact with them.”
Be honest with your medical team about vitamins or herbal supplements you’ve been taking in any form, whether pills, shakes, or powders. To educate yourself on herbs and potential adverse reactions or interactions with treatment, visit MSK’s About Herbs webpage.
If you’re overweight, aim for controlled weight loss.
With two-thirds of the American population classified as overweight or obese, many newly diagnosed cancer patients who fall into those categories consider the prospect of treatment-related weight loss to be a silver lining. But it’s not your ticket to become the Biggest Loser, Ms. Stella and Ms. Gerdes say.
“We want to make sure they’re not losing in an uncontrolled manner,” Ms. Gerdes says, noting that rapid weight loss usually involves the loss of lean muscle mass, which is needed to maintain strength. “Losing five to six pounds a week would be concerning.”
Use apps to keep track.
Since many patients already carry smartphones everywhere, Ms. Gerdes and Ms. Stella recommend using apps such as MyFitnessPal to keep an online food journal, tracking not only calorie intake and activity levels but also types of calories consumed.
“It’s a good visual for them, telling them how many carbs they’re getting compared to protein,” Ms. Stella says. “Since we’re always stressing protein, it really helps them see what foods are contributing to that and how they can improve their diet.”
“We only use mobile apps for weight loss,” she adds. “Using MyFitnessPal or mobile tracking devices are like having a dietitian with you at all times. It lets us know where a patient can make changes to their diet to eat fewer calories — which is the goal of tracking.”
After treatment, be prepared for change.
The end of treatment brings pivotal changes, both mental and physical, for cancer survivors, including a recommended switch back to a mostly plant-based diet to manage their weight. Just like other healthy people, survivors should follow the MyPlate recommendations to fill half their plates with fruits and vegetables and split the remaining half between grains and protein.
“For survivors, it’s still very important to make sure their weight is a healthy weight,” Ms. Gerdes says, explaining that this group may be at higher risk for other health conditions, including type 2 diabetes and heart disease. “We want to make sure that once they’ve gotten over the hump of treatment that they continue forward with a healthy diet, at a healthy weight, with a healthy lifestyle.”
Ms. Stella adds: “Recommendations about weight management are patient specific, and there is no meal plan that’s right for everyone. Patients undergoing active treatment will always be instructed to maintain or gain weight, while some survivors may be instructed to lose weight. It’s always best to check with your primary doctor to determine if weight loss, gain, or maintenance is best.”

