Three Memorial Sloan Kettering experts shared important research findings in plenary talks during Week 1 of the American Association for Cancer Research’s (AACR) virtual Annual Meeting 2021, held from April 10 to 15. Two presentations shed light on how genetic mutations lead to the development of cancer or promote its spread. A third reviewed new innovations in a promising form of cell-based immunotherapy.
Also at the 2021 AACR Annual Meeting, Matthew Matasar presented trial results on a potential new treatment for indolent B cell lymphoma.
Probing Chromosomal Chaos in Cancer Cells
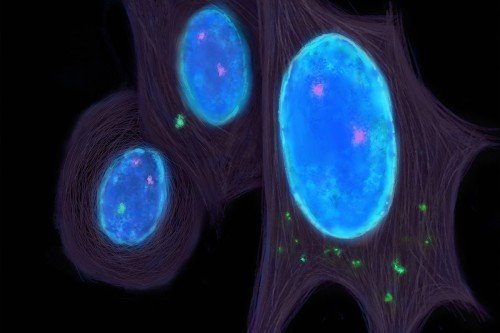
On April 10, physician-scientist Samuel Bakhoum spoke about chromosomal instability (CIN), a type of genetic chaos that is a hallmark of advanced and metastatic cancer. When cancer cells divide, DNA segments and even whole chromosomes are often duplicated, mutated, or lost altogether. Sometimes, bits of DNA from these chromosomes will end up where they don’t belong — outside of a cell’s central nucleus and floating in the cytoplasm.
Cells interpret these rogue bits of DNA as evidence of viral invaders, which sets off their internal alarm bells. This activates a warning system called cGAS-STING, which triggers inflammation and draws immune cells to the tumor site. But somehow, cancer cells not only survive the inflammatory environment but actually hijack cGAS-STING signaling to grow and spread.
Dr. Bakhoum’s laboratory in the Human Oncology and Pathogenesis Program (HOPP) investigates how CIN and cGAS-STING allow cancer cells to avoid immune defenses and metastasize. In his presentation, Dr. Bakhoum described how cGAS-STING signaling affects both the tumor and the surrounding tissues, blood vessels, immune cells, and noncancerous components (what’s called the microenvironment).
A 2018 discovery by the Bakhoum laboratory had shown that cGAS-STING signaling inside of cancer cells causes them to adopt features of immune cells — in particular, the capacity to crawl and migrate. This enables the cancer cells to slip away from the primary tumor and move to other parts of the body.
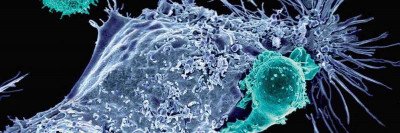
Dr. Bakhoum discussed his laboratory’s recent discovery showing how cancer cells cope with the warning signals that activated cGAS-STING releases into the environment. The cancer cells have a protein called ENPP1 on their surface that destroys cGAS-STING’s warning signals before they reach neighboring immune cells. In addition, ENPP1’s activity releases an immune-suppressing molecule called adenosine, which also quells inflammation.
Using mouse models of several cancers, Dr. Bakhoum and his colleagues showed that ENPP1 acts like a control switch for immune suppression and metastasis. Turning it on suppresses immune responses and increases metastasis; turning it off enables immune responses and reduces metastasis. Several pharmaceutical companies — including one that Dr. Bakhoum and colleagues founded — are developing drugs to inhibit ENPP1 on cancer cells.
ENPP1 is not the only mechanism that enables cancer cells with CIN to evade immune attack: Dr. Bakhoum’s team continues to probe for additional CIN-related vulnerabilities in cancer cells and has developed systems that enable genetic manipulation of CIN levels in tumors to probe the impact of chronic inflammation arising from cGAS-STING activation on the tumor microenvironment.
“While chromosomal instability was identified as a possible driver of cancer formation over a century ago, we have had very little understanding of how it actually causes tumor progression and metastasis,” Dr. Bakhoum says. “One of the most exciting developments over the past decade is our increased understanding of how chromosomal instability shapes the behavior of cancer cells and the immune cells in the tumor microenvironment.”
This is enabling researchers to develop new therapeutic strategies to selectively target tumors that have chromosomal abnormalities, he explains. “For over a century, chromosomal instability has been considered an undruggable black box — but now, we are starting to view it as an attractive therapeutic vulnerability.”
The Journey of a Blood Cell to Leukemia
In his presentation on April 12, physician-scientist Ross Levine focused on the genetic causes of leukemia at the level of single cells — specifically, how a series of mutations in normal blood cells can lead to them eventually becoming cancerous. “Leukemia is biologically complex with a wide range of prognoses from person to person, but it starts with a relatively small number of mutations,” Dr. Levine says.
A team led by Dr. Levine’s lab in HOPP made a major contribution to understanding this process in October 2020 in a large study spearheaded by postdoctoral fellows Linde Miles and Robert “Bobby” Bowman. The team deciphered mutations found in every single cell in samples from 146 people treated at MSK for acute myeloid leukemia (AML), as well as those with two blood conditions that can lead to AML: clonal hematopoiesis and a blood cancer called myeloproliferative neoplasms.
The analysis yielded data on nearly 750,000 unique blood cells and revealed how the mutations accumulate as the disease develops. Dr. Levine says the order in which these mutations occur, called the clonal architecture, can be compared to a family tree, with each branch taking the cells in a different direction. Some remain healthy, while others become aggressive cancer.
In his presentation, Dr. Levine explained how his team will take the new information about the clonal architecture back to the lab and use it to create more accurate disease models that can then be used to develop new ways to diagnose disease and potentially test new drugs. They recently received an Equinox Innovation Grant from Cycle for Survival to continue funding this research.
“We’re all playing a chess game against cancer, and this gives us a look into our opponent like we’ve never had before,” Dr. Levine says. “Think of each move as a therapeutic move, and now that we know more about what’s going to happen, we can stay one move ahead.”
No matter where you live, you can be part of the movement to beat rare cancers. There are many ways you and your friends and family can get involved, including a socially distanced outdoor ride at MetLife Stadium in New Jersey on May 1 and 2 and our first-ever virtual event experience on May 15. 100% of every dollar raised goes to rare cancer research led by MSK.
Register, donate, or learn more about cycleforsurvival.org »
Retooling CAR T Cell Therapy
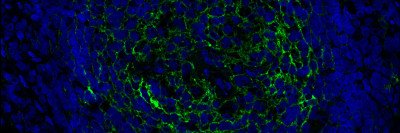
Physician-scientist Michel Sadelain, Director of the Center for Cell Engineering at MSK, spoke on April 14 about the latest strategies for boosting the effectiveness of chimeric antigen receptor (CAR) T cell therapy. MSK pioneered this treatment, which involves removing immune cells from a patient, arming them with synthetic proteins that allow them to recognize cancer, and returning them to the patient in large numbers. Often referred to as “living drugs,” CAR T cell therapy has already been approved for some blood cancers, such as certain types of leukemia and lymphoma.
CAR T cell treatment is still not completely effective, even in some people who initially respond well to the therapy. One limitation is that the T cells seem to lose their potency after a while, a phenomenon called T cell exhaustion that has hampered many types of cancer immunotherapy.
“There are intense efforts to understand what leads to this loss of T cell function, and at MSK, we are developing three approaches to address it,” Dr. Sadelain says. One tactic involves using the gene editing technology called CRISPR CAS-9 to deliver the gene for the CAR protein to a very specific location in the genome of the T cell. This precise approach creates CAR T cells with more stamina — they can kill tumor cells for longer. Another strategy is to modify the T cells’ epigenetic features — which relates to changes in gene activity that do not involve changes in their DNA sequence.
A third approach involves using a novel CAR design to enhance the power of the T cells so they are effective at a lower dose. It implements a new molecule called 1XX that improves CAR T cell effectiveness and prolongs their anticancer potency. This technology was created at MSK and currently has an open phase I clinical trial for people with B cell leukemia and lymphoma, led by hematologic oncologist Jae Park. Another trial, led by medical oncologist Roisin E. O’Cearbhaill, is testing 1XX-modified CARs in people with pleural mesothelioma, a cancer that develops in the thin tissue lining the lungs.
A second major limitation of CAR T therapy is that the T cells often cannot eliminate cancer cells that have very low levels of the cancer antigen that they have been engineered to target and destroy — a problem known as “antigen escape.” MSK researchers have developed a technology that incorporates a molecule called a HIT receptor into T cells. The T cells armed with HIT can detect much lower antigen levels. MSK just got funding to start a trial testing HIT within the next year or so.
Although these technologies are still in an early stage, Dr. Sadelain expects his presentation on 1XX and HIT to attract great interest in the CAR T field.
“The present evolution of CAR T cell manufacturing is informed by meticulous analyses of how T cells are wired and what receptors make them work,” he says. “It’s not just an academic discussion of mechanisms — it aims to push the limits of our immune system and will impact many clinical trials. Ultimately, it will make this revolutionary form of immunotherapy even more effective for patients.”