Let's get started
World-class experts. Close to you.
Many treatments and services are available at locations across NY and NJ.
Get care from the comfort of your home with telemedicine from MSK.
Explore MSK’s clinical trials
Our doctors and scientists work together so patients get access to cutting-edge treatments as soon as they are available.
Cancer news & discoveries
Article
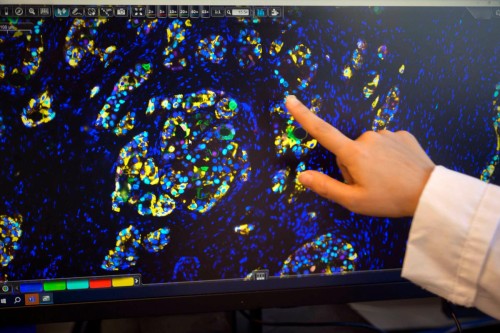
Making Progress Against Metastasis
While there has been remarkable progress in the number of people surviving with stage 4 cancer, MSK remains dedicated to research that will spur much needed advances.
Read more

Article
New Colorectal Cancer Treatments at MSK Aim To Reduce Deaths in 2026 and Beyond
Learn about the latest treatments for colon and rectal (colorectal) cancer at Memorial Sloan Kettering Cancer Center.
Read more

Article
Reasons Why MSK Is a Leader in Stem Cell and Bone Marrow Transplants
Dr. Miguel-Angel Perales explains why MSK has continued to be a leader in the field of stem cell and bone marrow transplantation for more than 50 years.
Read more




