
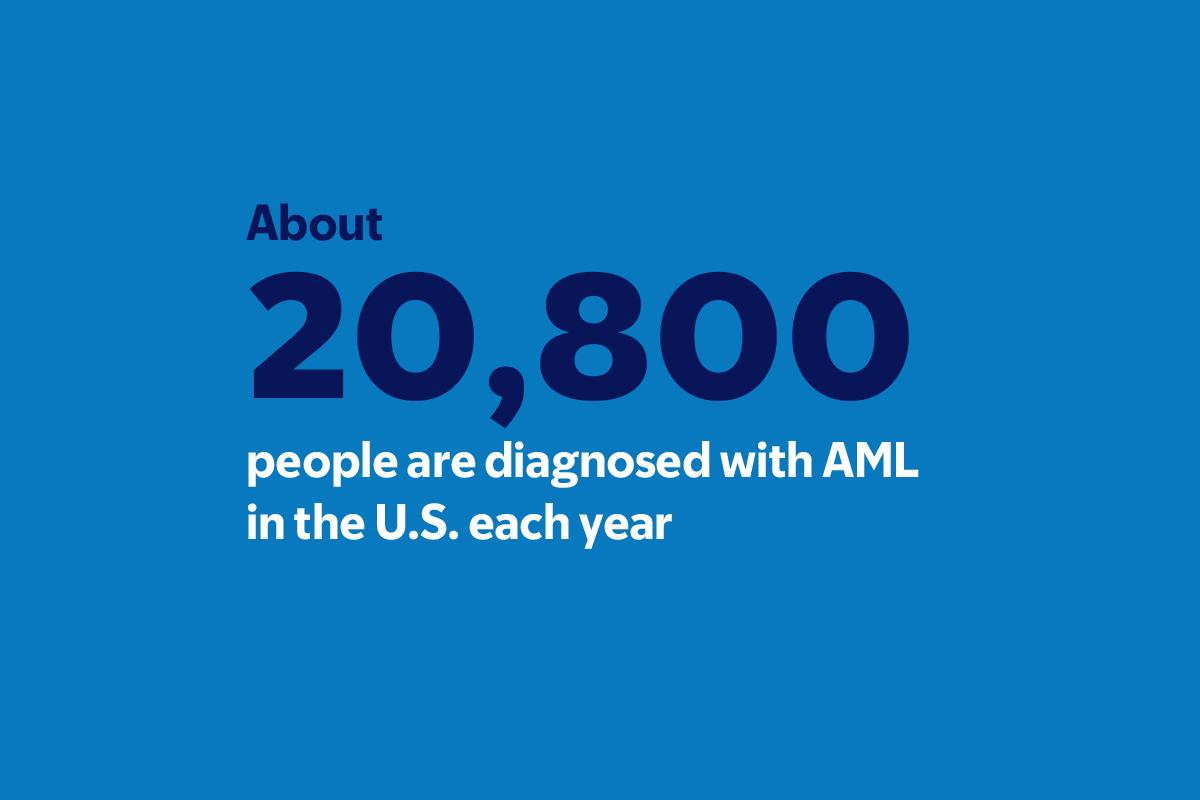
Ever since he was in college, Michael Rosensweig has endured a series of grueling treatments for acute myeloid leukemia (AML). This kind of blood cancer is relentless. It moves quickly and needs aggressive, often harsh, treatment with chemotherapy, sometimes followed by a bone marrow transplant. Even when these therapies stop the cancer, AML often returns.
Then Michael found out that he qualified for a groundbreaking clinical trial of an experimental targeted therapy.
“I’ve been through a lot,” says Michael, now 35 and a software engineer living in Manhattan. “But I’m still here and more hopeful than ever.”
The outlook for Michael and other AML patients has begun to improve dramatically, thanks to research in laboratories and clinics at Memorial Sloan Kettering Cancer Center (MSK) focused on conquering the cancer’s major challenge: AML has many subtypes, with an array of genetic mutations driving the cancer.
“We now have a much better understanding of what drives this disease,” says hematologic oncologist Eytan Stein, MD, Director of the Program for Drug Development in Leukemia. “It’s an amazing, exciting time to be doing leukemia research.”
In the past few years, several new targeted therapies are showing remarkable results. One new drug, venetoclax (Venclexta®), is effective in older people when combined with another therapy. In addition, MSK’s Leukemia Service led trials that resulted in the approval of two drugs by the Food and Drug Administration — enasidenib (Idhifa®) and ivosidenib (Tibsovo®).
A New Class of Drugs To Treat AML
In 2023 came perhaps the biggest breakthrough of all: proof that a new class of drugs known as menin inhibitors could stop the most lethal form of AML. It was the culmination of research begun a decade ago in the labs of leukemia oncologist Ross Levine, MD, MSK’s Deputy Physician-in-Chief for Translational Research, and Scott Armstrong, MD, PhD.
That groundwork paved the way for a phase 1 clinical trial led by Dr. Stein and published in Nature, which showed that a menin inhibitor called revumenib was effective in people whose cancer had certain molecular mutations common in AML:
- More than half of these patients responded to revumenib.
- About 30% had a complete response with partial hematologic recovery, which means that no cancer was detectable in their blood.
“People with these types of alterations tend to have the most dangerous type of this already tough disease,” Dr. Stein says. “What we’ve seen in this study is very promising.”
Another Chance for Michael
When Michael participated in the clinical trial in 2021, his AML had returned three times since he was a junior at the Massachusetts Institute of Technology.
Michael feared he had run out of chances. But Dr. Stein’s groundbreaking trial gave him the opportunity to avoid another round of intensive chemotherapy requiring weeks of hospitalization. Instead, he could take a pill at home twice a day for four weeks.
“Being able to do treatment from home and just be normal for a while was so nice, as opposed to being stuck in a hospital bed for months,” Michael says.
Engineering the Immune System To Fight AML
Researchers are also making inroads treating AML with chimeric antigen receptor (CAR) T cell therapy. This treatment involves removing T cells from a patient and outfitting them in the lab with receptors that recognize specific targets — known as antigens — on the surface of a cancer cell. When these modified cells are put back into the patient, they patrol the bloodstream looking for cancer cells to destroy.

But AML is a wily enemy. Its cells have different target antigens from cell to cell. So CAR T therapy could inadvertently weaken the entire immune system, requiring the patient to have a “rescue” bone marrow transplant.
Physician-scientist Michel Sadelain, MD, PhD, a pioneer in CAR T cell research, has developed an ingenious tactic for solving that problem in mice, reported in Cancer Cell. His team designed CAR T cells that activate into supercharged killing mode only if they sense two particular AML antigens at sufficient levels. These antigens — ADGRE2 or CD371 — can be present even at low levels, and the CAR T cells are still potent against them, without causing severe side effects.
A clinical trial using this approach is now beginning under the direction of hematologic oncologist Jae Park, MD.
As for Michael, thanks to the menin inhibitor, he was able to receive a bone marrow transplant. Now cancer free for two years, he says, “I’ve got my life back and I’m so grateful.”
This research receives essential philanthropic support from the MSK Giving community, including Cycle for Survival®, Mazumdar Shaw Philanthropy, Lewis A. Sanders, and Wendy and Neil Sandler (Dr. Sadelain); Fred’s Team® (Dr. Stein); and Comedy vs Cancer (Dr. Park).
Dr. Levine holds the Laurence Joseph Dineen Chair in Leukemia Research.
Dr. Sadelain holds the Stephen and Barbara Friedman Chair.