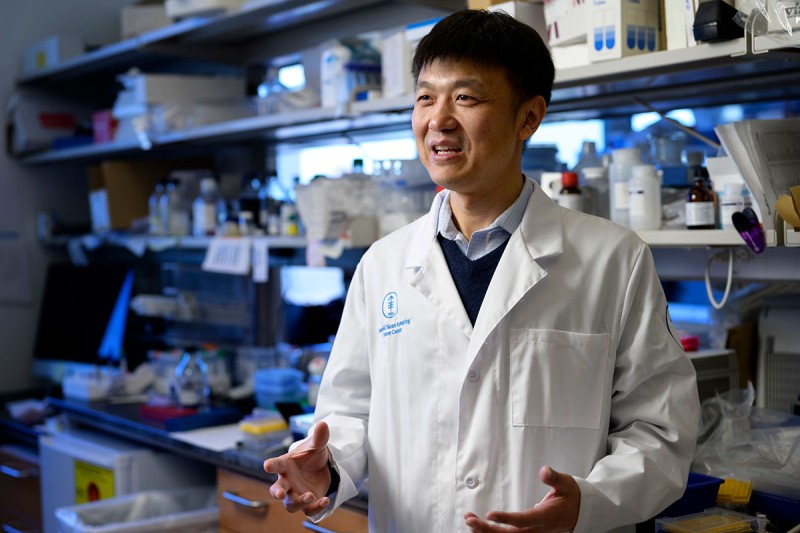
Investigator Ming Li, PhD, has dedicated his career to understanding the intricate workings of the immune system — both in general and for the critical role it plays in cancer.
Study by study, his lab at Memorial Sloan Kettering Cancer Center (MSK) is sharing new insights into the molecular and cellular mechanisms involved in immune regulation — a type of knowledge-building that scientists call “basic science” or “discovery science.” But Dr. Li is equally focused on applying that knowledge to harness the power of the immune system against cancer.
“Immunotherapy has become a really important area in cancer research,” says Dr. Li, a member of the Immunology Program at the Sloan Kettering Institute, a hub for basic and translational research within MSK. “The idea that we can engage the immune system to control cancer is something that many cancer biology labs are now pursuing.”
For example, in a new study in Immunity, one of the top immunology journals, Dr. Li and his colleagues describe a tumor suppression pathway they believe could form the basis for a new immunotherapy approach.
We recently sat down with Dr. Li to discuss the new findings and his research program at MSK.
What are the big questions your lab is trying to answer to understand the immune system and make cancer immunotherapy more effective?
First and foremost, we are interested in how the immune system is regulated at a mechanistic level. That means doing experiments to understand in precise detail the mechanisms by which immune cells interact and coordinate to mount an immune response against threats to an individual’s health.
Cancer cells pose a unique challenge for the immune system. They are a person’s own cells, but they can act like foreign invaders. And cancer has ways of hijacking the immune system for its own benefit.
How the immune system recognizes bacteria and other infections has been well studied. But how it recognizes a healthy cell that’s transforming into a cancer cell is still a relatively new discipline.
I started my lab in 2007, and over the past 16 years we’ve investigated the diverse ways that the immune system perceives and responds to cell transformation.
During this same period, the development of immunotherapy has revolutionized cancer treatment worldwide — that is, tapping into the power of a person’s immune system to fight against their cancer. When it works, it can have amazing results. The challenge is making it work for more people and more types of cancer.
In my lab, we’re uncovering new biological insights with the aim of doing exactly that.
Tell us about some of the important discoveries from your lab and how they might inform future therapies.
I think our work has helped to expand ideas about how we might go about targeting the immune system for cancer therapy.
My lab is primarily focused on a type of white blood cells called lymphocytes, including T lymphocytes. T cells recognize abnormal cells and target them for destruction. They play a central role in the immune response that is known as “adaptive,” because it learns to identify the invader and can remember how to attack it.
We discovered that a type of adaptive T cells called “helper T cells” are regulated by the TGF-beta pathway to control the tumor immune response. Blocking TGF-beta signaling in helper T cells creates a defensive response that could be used against cancer. This approach underscores the idea of targeted immunotherapy approaches for complex regulators such as TGF-beta.
Today, adaptive lymphocytes are the main focus of programs to develop checkpoint inhibitor therapies, to which the helper T cell-directed TGF-beta blockade belongs. But we discovered that two additional types of tumor-resident lymphocytes called “type 1 innate lymphoid cells” and “killer innate-like T cells” play an important role in cancer immune surveillance. That’s the process by which the immune system detects and eliminates newly transformed cancer cells to prevent the development of tumors.
Our first paper on this topic was published in 2016, and we’ve had several additional follow-up studies that took our initial findings in mouse models into a human context, and identified interleukin-15 as a pivotal regulator of these newly discovered cancer immune surveillance responses. These include recent papers in Nature, Nature Immunology, and Science Immunology.
We are optimistic that the ability to activate these tissue-resident innate lymphocytes and innate-like T cells could be developed into a next-generation immunotherapy.
Meanwhile, there’s a whole separate arm of our research program that is looking at the role of macrophages in cancer. Macrophages are a different type of white blood cell that engulfs and digests invaders, like bacteria and cancer cells.
Macrophages play a complicated role in cancer because macrophages found in and around tumors — what we call tumor-associated macrophages — can actually support tumor growth.
We published a paper this summer in Nature that showed tumor-associated macrophages can be reprogrammed to outcompete certain cancer cells for resources. And these findings suggest that this pathway might be harnessed against aggressive cancers that are fueled by cell competition.
What about the new study, what did it reveal about the role of macrophages in cancer?
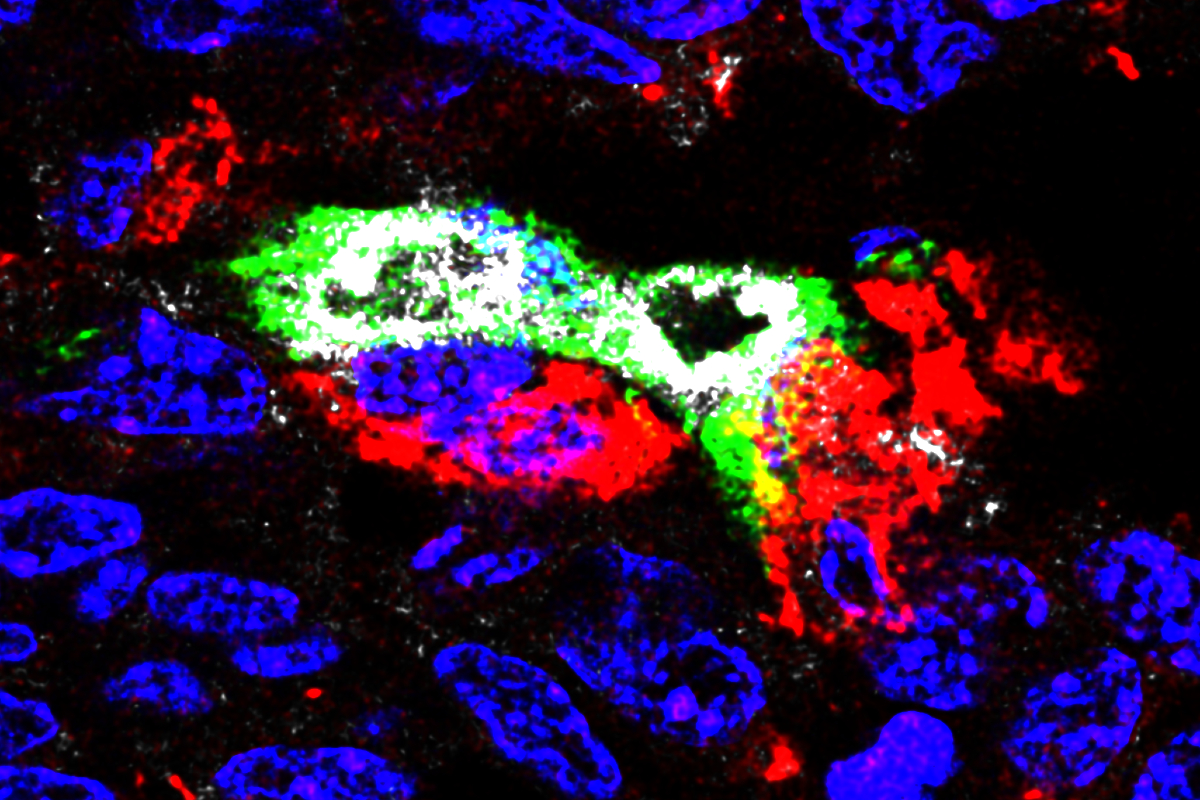
The new study in Immunity was also one that focused on tumor-associated macrophages, which we call TAMs for short.
The work — which was co-led by former lab members Mytrang Do, MD, PhD, and Wei Shi, PhD, and current postdoc Liangliang Ji, PhD — showed how tumors make a favorable environment for their growth by promoting the infiltration of TAMs into the tumor.
Using a mouse model of breast cancer, we found that TAMs found inside tumors had low activity of a key metabolic regulator called mTORC1. We also found that depleting a protein that blocks mTORC1 activity in these cells helped to reduce tumor growth by blocking blood vessel growth and cutting off cancer cells from access to oxygen.
So we see this as another opportunity to harness the power of the immune system to fight cancer — in this case, by increasing mTORC1 signaling within these tumor-associated macrophages to prevent the generation of a supporting tumor tissue blood vasculature.
Ultimately, we believe there’s great hope for precision immuno-oncology — that is, using the diverse immunotherapy weaponry tailored to the specific cancer threat of an individual patient. This is a very exciting time in immunotherapy discovery, and I’m privileged to be able to contribute to making immunotherapy work better and for more people.
Disclosures
MSK has filed patent applications regarding targeting mTORC1 signaling pathways in macrophages and IL-15 pathways in innate lymphoid cells and innate-like T cells, and also for targeting TGF-beta signaling in helper T cells for cancer immunotherapy. Dr. Li is a Scientific Advisory Board Member of and holds equity or stock options in Amberstone Biosciences and META Pharmaceuticals.