Memorial Sloan Kettering researchers are unceasingly searching for better ways to treat colorectal cancer, a disease that causes close to 700,000 deaths worldwide each year. One area of particular interest has been a gene called APC, which is mutated in up to nine out of ten colorectal tumors.
Scientists have known for some time that APC mutations, which shut down the gene’s normal activity, can cause the formation of colorectal cancers. But thus far they haven’t been able to tell whether the same gene changes continue to play a role in more-advanced tumors.
Now, for the first time, an MSK study published in the journal Cell shows that APC mutations spur the progression of the disease, suggesting the gene might be a promising target for future drugs. Working in mice, our researchers found that by artificially restoring the gene’s activity — essentially undoing the effect of an APC mutation — it’s possible to revert colorectal cancer cells back to normal and prevent the cancer from returning.
“The results of this study are just really clear cut,” says Cancer Biology and Genetics Program Chair Scott Lowe, who led the research. “It tells us a lot about colorectal cancer from a biologic perspective, and it has important ramifications for potential therapies.”
A Mouse Model Based on RNA Interference
In the study, the researchers developed a new mouse model of colorectal cancer. They engineered the mice using a technology called RNA interference (RNAi), which allowed them to switch off the APC gene and induce colorectal tumors that replicate key features of the disease seen in patients.
In mouse models scientists have used previously to study the disease, the gene was permanently removed, or “knocked out,” Dr. Lowe explains. “Deleting the gene could tell us that APC mutations can lead to cancer, but it couldn’t tell us what restoring APC would do. Once the gene’s gone, you can’t put it back.”
In contrast, when genes are shut down using RNAi technology, their activity can be turned back on. When the researchers restored the expression of APC in the mice, they were surprised by the dramatic effect. Within four days, tumors stopped growing and the mice regained normal intestinal function. After several weeks, all tumors had regressed, and months later the animals’ cancer hadn’t returned.
Making Colorectal Cancer Cells Normal
“What was even more surprising to us was that restoring APC appeared to transform tumor cells and make them seemingly normal again,” Dr. Lowe notes. “It wasn’t that the cells died or stopped dividing. They seemed to return to their original, noncancerous state and were able to function normally.”
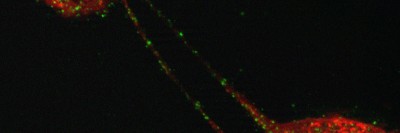
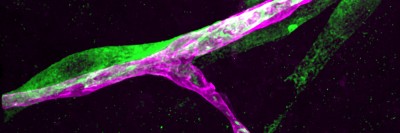
For example, the researchers performed experiments using intestinal organoids — small, three-dimensional structures of cells derived from the intestinal glands of mice. The cells within the organoids, which grow together in a way that resembles their natural tissue arrangement, can be used as a tool to study how gene changes may affect colorectal cancer biology.
“When we used RNAi to silence APC, the organoids lost their normal shape and formed spheres, which is typical of how cancer organoids grow,” explains Kevin O’Rourke, a graduate student in our Tri-Institutional MD-PhD program who served as the study’s first author along with research fellow Lukas Dow. “And when we reactivated APC expression, this restored normal cell division and growth.”
Hints for Future Therapy
The APC gene controls a biological process called the WNT pathway, which is deactivated in most colorectal tumors. The findings suggest it might be possible to develop a new type of drug that reactivates the pathway in colorectal cancer cells.
Such a potential therapy might work against a broad range of APC-mutated tumors, including some that contain additional mutations. In the study, the researchers found that restoring APC expression could also effectively treat mice whose colorectal tumors carried mutations in the genes Kras and p53 — which are found in about half of patients with colorectal cancer.
Dr. Lowe emphasizes that developing a new drug and determining its long-term clinical value could take years. “Earlier studies have shown that completely blocking the WNT pathway could be severely toxic to normal intestinal cells and lead to side effects,” he says. “But our findings suggest that small molecules that have been carefully designed to modulate the pathway — as opposed to blocking it — might achieve effects in patients similar to those we’ve seen when reactivating APC expression in our mouse model.”