Acute myeloid leukemia (AML) is one of the most challenging blood cancers. The disease moves quickly and needs aggressive treatment with chemotherapy, sometimes followed by a bone marrow transplant. Even when the first round of therapy works, AML often returns.
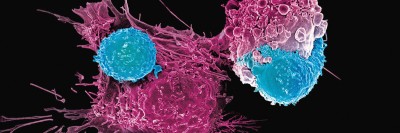
Now a clinical trial at Memorial Sloan Kettering Cancer Center (MSK) offers hope for a new way to treat this relentless disease. The investigational approach uses chimeric antigen receptor (CAR) T cell therapy. This form of immunotherapy involves removing T cells from a patient and outfitting them in the lab with receptors that recognize specific targets — known as antigens — on the surface of a cancer cell.
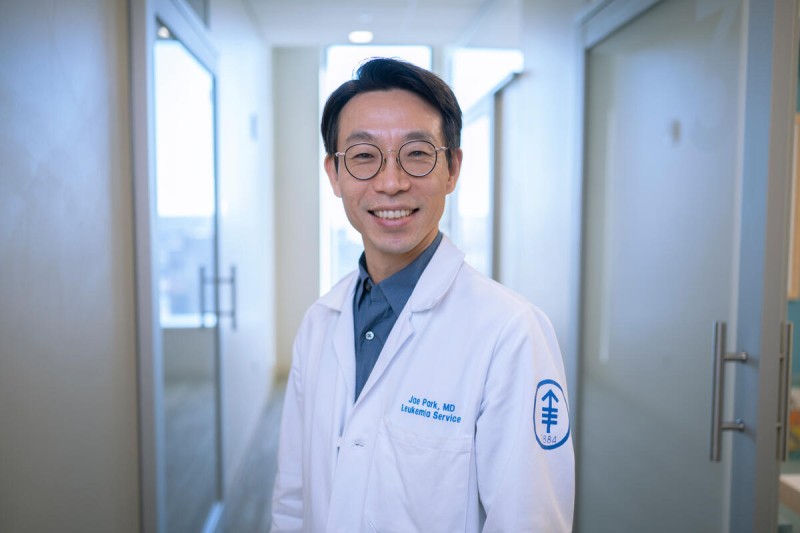
The phase 1 trial, led by hematologic oncologist Jae Park, MD, is the result of groundbreaking research from the laboratory of physician-scientist Michel Sadelain, MD, PhD, a pioneer in CAR T research. Dr. Sadelain’s team published results in Cancer Cell in October 2023, showing that a new type of CAR T cell could selectively destroy AML cells in mice without causing toxic side effects. The CAR T cells target two antigens at once.
“It’s been very challenging to develop good AML treatments, including effective CAR T therapies,” Dr. Park says. “Michel’s lab research on this CAR T design has been building toward this for years, and it’s great we can finally study it in people.”
In the trial, researchers will try to determine the best dose of the therapy that can be used safely in people with AML who have resisted other treatments. Researchers will also analyze samples from the patients to look for signs that the CAR T cells are attacking the cancer.
Why AML Has Resisted Previous CAR T Therapies
The complex makeup of AML has complicated previous efforts to use CAR T therapies. Even within the same patient, AML cells can have different antigens expressed at different levels from cell to cell. This makes it difficult to design an effective therapy that targets just one antigen.
In addition, AML cells share antigens with normal blood stem cells, which give rise to all cells of the blood — including immune cells. Therefore, conventional CAR T therapy targeting AML could inadvertently decrease blood production or weaken the entire immune system. This would require the patient to have a “rescue” bone marrow transplant even if the treatment worked.
The challenge has been to develop CAR T cells that are powerful enough to detect even a low level of an antigen in the AML cells, while sparing the normal blood stem cells.
In the New Clinical Trial, CAR T Cells Attack Two Targets at Once
Dr. Sadelain’s lab developed an ingenious approach to create a CAR T cell that is just strong enough. Working with senior research scientist Sascha Haubner, MD, his team designed CAR T cells that detect two antigens at once: ADGRE2 and CLEC12A. Only AML cells have the combination of both antigens present at detectable levels. When the CAR T senses both antigens, it activates and kills the cell. If it detects neither antigen — or just one — it holds its fire.
“In recent years, our lab has been fine-tuning CAR T cells to be more sensitive to target antigens so that cancer cells cannot escape the attack if antigen levels are low,” Dr. Haubner says. “But this increased power of the CAR T cells is also a threat to normal cells sharing the antigen. By designing the CAR T cells to look for cooperative signaling from two target antigens, we could keep the CAR T cell potency high while minimizing its damage to normal cells.”
Dr. Sadelain’s team selected ADGRE2 and CLEC12A as the target antigens by analyzing samples from patients with resistant AML and doing a series of tests in mouse models beginning in 2018. They showed that CAR T cells designed for these antigens were safe and effective against human AML cells implanted in mice. Based on these results, the clinical trial was approved to go forward.
“We were convinced we would be able to test this in people, and we were helped by Michel’s expertise and MSK’s experience in doing first-in-human trials to get approval for the trial,” Dr. Haubner says.
Dr. Park expects very high interest in the trial from patients. If results from the first six patients are encouraging, the trial might expand to include more people. For now, he’s optimistic this new approach could open the door to similar therapies for other cancers.
“This is an exciting development that has the potential to change the outlook for AML patients who previously had little to no hope,” Dr. Park says.