
A new imaging technique developed at Memorial Sloan Kettering Cancer Center (MSK) shows promise for detecting deadly forms of lung cancer and prostate cancer. The technology uses a radioactive particle that binds to a ligand (molecule) on cancer cells called DLL3, making the cells more visible on PET scans.
The DLL3 ligand is especially prominent in small cell lung cancer (SCLC) and neuroendocrine prostate cancer (NEPC), which are aggressive types of the disease.

Detecting these cancers would help identify patients who might respond well to a new class of drugs that target DLL3.
Many of these therapies are already showing potential in clinical trials. Scientists are also making progress on delivering these drugs along with the radioactive substance — a combination that would act as a therapeutic smart bomb to target the cancer cells and leave normal cells unharmed.
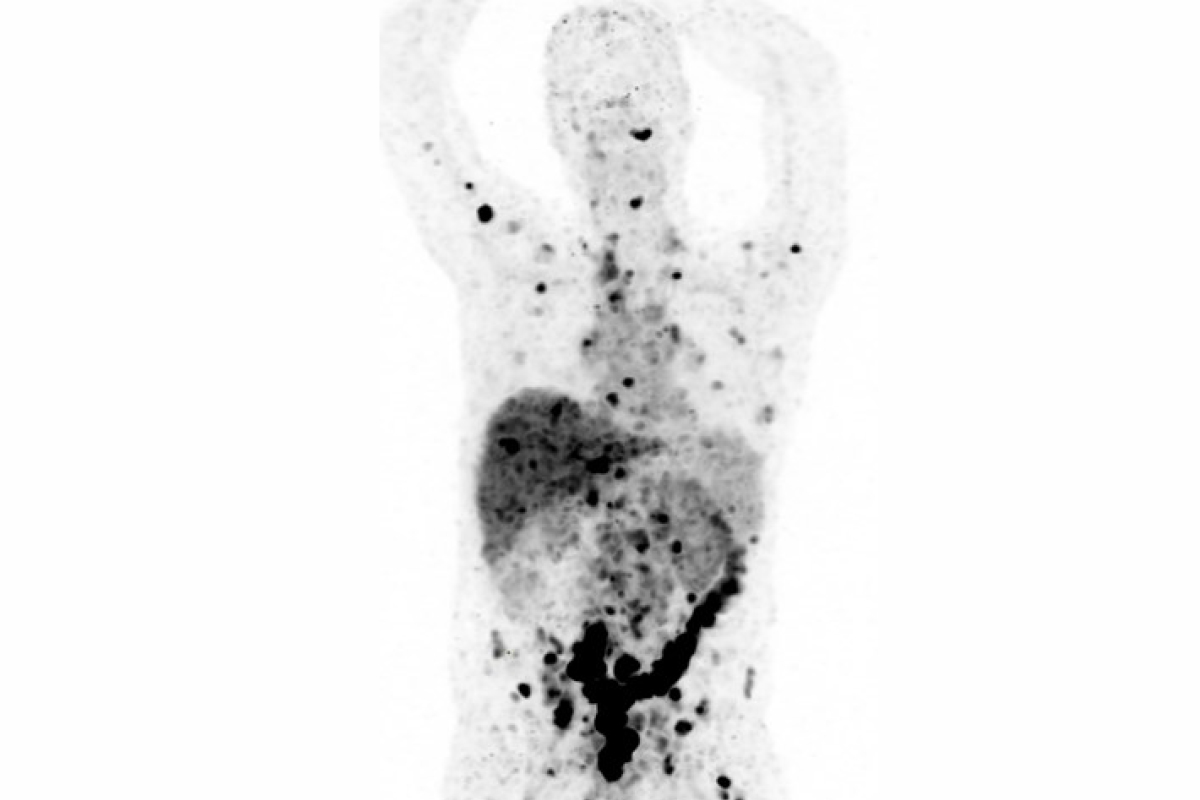
Results from the first pilot study, published in The Lancet Oncology, show that the imaging agent reliably detected cancer cells containing DLL3 in 18 patients. There were no safety concerns, and researchers are already planning to test the radioactive agent in a larger group.
An accompanying commentary in the journal called the research “a pivotal milestone” that is “notable for its scientific novelty and the potential to improve patient outcomes.”
Targeting DLL3 in SCLC and NEPC May Help Improve Treatment Outcomes
The imaging agent, called [89Zr]Zr-DFO-SC16.56, was developed in the laboratories of MSK radiochemist Jason S. Lewis, PhD, and physician-scientist Charles M. Rudin, MD, PhD. The substance is injected into the body by a nuclear medicine physician. Over the next few days, it’s absorbed by cancer cells containing DLL3. The nuclear medicine physician can then read the PET scan to see the extent of the cancer and make treatment decisions.
“About 70% to 80% of small cell lung cancers express DLL3 at various levels,” Dr. Rudin says. “In the short term, this technology could be essential for finding out whether a patient should receive a DLL3 drug or a different therapy. And, if we can link the imaging agent to drugs or therapeutic isotopes, we would have an important new treatment option for these cancers.”
MSK has been awarded multiple grants to continue developing and validating the DLL3-based technology — most notably an $8 million grant from the Prostate Cancer Foundation to Dr. Lewis and his colleagues.
Nuclear medicine physician Lisa Bodei, MD, PhD, who is Director of Targeted Radionuclide Therapy at MSK, is working with nuclear medicine physician Mark Dunphy, DO, and Dr. Rudin to develop and test other radioactive therapies. They are collaborating with Salomon Tendler, MD, PhD, a research fellow in Dr. Lewis’s lab and the first author of the Lancet Oncology study.
The Importance Of Diagnosing Small Cell Lung Cancer and Neuroendocrine Prostate Cancer
SCLC and NEPC are neuroendocrine cancers, which develop in cells that produce hormones.
Small cell lung cancer tends to spread quickly to other areas and to the lymph nodes in the chest. The five-year survival rate is 18% if it has already spread outside the lungs at diagnosis.

Neuroendocrine prostate cancer is rare but very deadly with no effective standard therapy. It can arise as a new cancer (called “de novo”). Other times, it results when the more common form of prostate cancer, adenocarcinoma, transforms into NEPC — often in response to treatments such as hormone therapy or chemotherapy.
“NEPCs are difficult to detect and diagnose without biopsies and have become an increasing problem in prostate cancer patients,” Dr. Rudin says.
The new technology could also pick up metastatic SCLC and NEPC that more conventional imaging might miss. Dr. Rudin says the new imaging agent can detect small cancers that have spread to the brain. It also may work for imaging other cancers such as thyroid cancer or neuroblastoma.
Building on Success in Theranostics for Lung and Prostate Cancer
The new imaging agent represents another important advance in the emerging field of theranostics. This area of medicine uses radioactive substances to see cancer cells as well as carry therapies to destroy them without harming normal cells.
MSK has already had success in this burgeoning field. In 2022, the U.S. Food and Drug Administration approved a similar theranostics treatment called 177Lu-PSMA-617. This treatment targets a protein in prostate cancer cells called PSMA (prostate-specific membrane antigen). MSK genitourinary oncologist Michael Morris, MD, helped design, execute, and analyze a clinical trial showing the effectiveness of 177Lu-PSMA-617 in people with metastatic prostate cancer.

“DLL3-targeting technology could be the next generation of theranostics, guiding new treatments for patients with small cell lung cancer or neuroendocrine prostate cancers who otherwise would have run out of options,” Dr. Lewis says.
Dr. Dunphy added it’s important to develop multiple imaging agents that target different proteins on cancer cells.
“A lot of radioactive treatments stop working after a while — often the cancer starts to evolve, and the target disappears,” he says. “For example, 177Lu-PSMA-617 can find and treat prostate adenocarcinoma, but if the disease transforms into neuroendocrine prostate cancer, the tumors will likely lose the PSMA target and no longer absorb the radioactive drug.”
How Team Brainstorming Pushes Lab Discoveries into the Clinic at MSK
Drs. Rudin and Dunphy say MSK offers a unique opportunity for collaboration between basic scientists and clinicians.
“It’s amazing to have the kind of research meetings where all the parties are sitting together,” Dr. Dunphy says. “We have incredible radiochemistry experts who talk about how to design new imaging technologies. And then our oncology experts will say, ‘Don’t chase after that one. Here’s what is clinically relevant to us.’ There’s this constellation of stellar investigators brainstorming a realistic vision of the future.”