Lung cancer was one of the first cancers that could be targeted by drugs aimed at specific mutations in tumors. Advances in genomic medicine and the molecular analysis of tumors can largely take the credit for this early progress. Unfortunately, that also means that people with lung cancer who were treated with these drugs were among the first to develop resistance. When a treatment that initially works stops working, it is called acquired resistance. Overcoming acquired resistance is one of the most critical challenges in cancer research today.
Memorial Sloan Kettering investigators are at the forefront of studying this problem. They are looking for ways to address acquired resistance. The methods they are considering include combination therapies that attack cancer on multiple fronts at the same time.
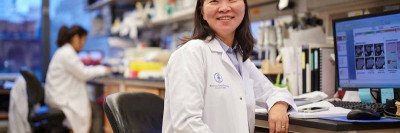
“We’re taking personalized medicine to the next level — version 2.0,” says MSK medical oncologist Helena Yu. “It’s not enough anymore to just look for a mutation and give everyone who has the mutation the exact same treatment. Many factors influence how people respond to therapy, and we’re trying to direct treatment in a much more specialized way.”
Is Treatment Resistance Inevitable?
About 20% of lung adenocarcinomas, the most common lung cancer in the United States, are driven by mutations in a gene called EGFR. This type of cancer is often found in people who have never smoked. The first targeted therapy to treat EGFR-driven cancer, called gefitinib (Iressa®), was approved by the US Food and Drug Administration in 2003. Since then, these drugs have become a conventional treatment. As a result, testing for EGFR mutations has become a standard part of diagnosis for advanced lung cancer.
Most people who take these drugs benefit greatly from them. Their tumors shrink measurably, leading to an improvement in some cancer symptoms, such as pain and shortness of breath. In addition, EGFR inhibitors are taken at home as pills and have few side effects compared with chemotherapy.
But the effectiveness of EGFR inhibitors is not long lasting. Although some people respond for years, the average time until the drugs stop working is 12 to 18 months. In some people, the drugs work for only a few months or not at all.
“Not all of the cells within a tumor are the same,” Dr. Yu says. “Even if 99% of the cells respond to an EGFR inhibitor and die off, the ones that don’t die will eventually become dominant and start to take over. Also, because cancer is a living thing, it has the ability to evolve and adapt while being exposed to treatment.”
Finding Genetic Markers for Resistance to Targeted Drugs
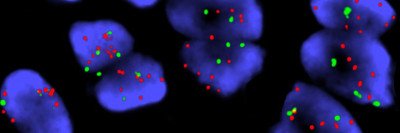
When people with lung cancer stop responding to an EGFR inhibitor, their MSK doctors are ready with an arsenal of other treatments. Many patients have a second biopsy. The resistant tumor is then analyzed with MSK-IMPACT™, a test that looks for more than 400 mutations that are known to play a role in cancer.
“Sometimes we find a mutation that wasn’t there the first time we analyzed the tumor. That may suggest that there are other targeted drugs to try,” Dr. Yu says. But other acquired changes, such as changes that don’t affect genes’ sequences, are not detected with MSK-IMPACT.
“Genomic sequencing of tumor tissue is part of the story, but not the whole story,” she adds. “We’re working on additional tests that can detect other kinds of molecular changes.”
MSK investigators are also developing liquid biopsies. These tests could allow doctors to analyze the molecular changes in a tumor with a blood test rather than having to take samples of the tumor from the lung.
Combining Targeted Therapies for a One-Two Punch
MSK already has clinical trials underway to address some of the acquired mutations commonly seen in lung cancer. One clinical trial combines a newer EGFR inhibitor called osimertinib (Tagrisso®) with an experimental drug called AZD6094. This second drug targets a mutation in the gene Met. About 20% of people treated with osimertinib eventually develop a Met mutation.

Another trial is looking at the combination of osimertinib and bevacizumab (Avastin®). Bevacizumab blocks the growth of a tumor’s blood vessels. Earlier research suggested that it is sometimes effective in combination with EGFR inhibitors.
Researchers have found that EGFR inhibitors can drive some adenocarcinomas to transform into small cell lung cancer, a type of lung cancer that is treated with different drugs. And so another trial is testing osimertinib in combination with the chemotherapy drugs typically used to treat small cell lung cancer. This trial is open to people whose tumors carry genetic mutations that make their cancer more likely to transform. “We’re always trying to stay ahead of the curve,” Dr. Yu says.
Most people with EGFR mutations don’t initially respond to immunotherapy, but they may respond if the cancer develops additional mutations.
Dr. Yu emphasizes that combination treatments have more side effects than using EGFR inhibitors on their own. That is why it is important to carefully identify who is likely to benefit from these more aggressive drugs.
“Unfortunately, we can’t cure stage IV lung cancer as of yet, but the longer we can maintain people on treatments that are effective and have minimal side effects, the better,” she concludes. “We want to be able to stretch out the benefit for each treatment as long as possible while, at the same time, always having more options in our back pocket when we need them.”