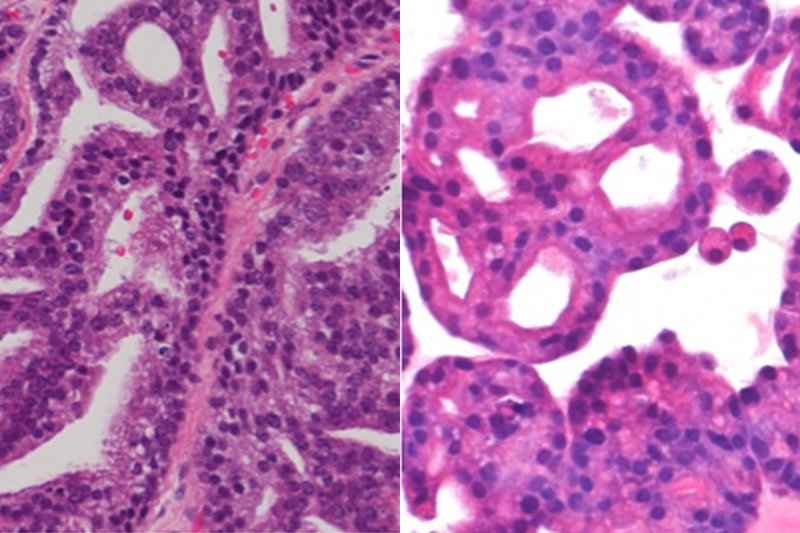
An international team of researchers led by Memorial Sloan Kettering has created a new tool that can be employed in the search for personalized cancer therapies in prostate cancer: tiny formations called organoids. The study of organoids — three-dimensional structures about a millimeter in size composed of cells grouped together and spatially arranged like an organ or tissue — is a rapidly growing field in biology.
Traditionally, cell lines have been one of the main resources for evaluating potential new cancer drugs in the lab. Cell lines are populations of cells derived from a patient — such as a cancer cell — that can be grown indefinitely in culture.
“Identifying the molecular biomarkers that indicate whether a drug will work or why a drug stops working is paramount for the precision treatment of cancer,” says Yu Chen, the study’s senior author and a physician-scientist in MSK’s Genitourinary Oncology Service and our Human Oncology and Pathogenesis Program (HOPP). “By developing these organoids from patient prostate cancer samples, we are able to study the tumors in greater detail and correlate the genetic mutations with the response to various drugs.”
Organoids are also expected to provide much more information than cell lines. Because organoids mimic the structure of tumor tissue, they will enable the study of how the cancer cells interact with each other and the effect of hormones on tumor growth, for example, in addition to providing genetic markers for targeted drug therapies.
A Need for Better Prostate Cancer Models
Despite prostate being the most common type of cancer in men after skin cancer, until now there have been only a handful of prostate cancer cell lines available for testing of new drugs. “Many of the mutations that cause prostate cancer occur in a small percentage of patients and are not represented at all in the cell lines currently available,” Dr. Chen explains. “And with so few lines, we haven’t had the statistical power to properly evaluate targeted therapies that may act against these mutations.”
In the new study, published in Cell, the researchers reported successfully growing organoids from the tumors of seven patients with metastatic prostate cancer. Each three-dimensional organoid is molecularly identical to the patient’s cancer from which it originated. With the addition of the seven organoid lines described in this paper, Dr. Chen’s team has effectively doubled the resources available for doing this kind of testing of new prostate cancer drugs.
A New Era of Personalized Medicine
The organoids are proving useful in learning more about the effectiveness of current and experimental prostate cancer therapies. The prostate cancer organoids can be used to test multiple drugs simultaneously, through a technique called high-throughput screening.
Eventually, the researchers say, they may be able to develop organoids that are derived from each patient’s tumor, allowing drugs to be tested on the organoid before being given to the patient to truly personalize and optimize each person’s treatment. Dr. Chen’s team is already retrospectively comparing the drugs given to each patient against the organoids for clues about why the patient did or didn’t respond to therapy.
An Exploding Field
The use of organoids in studying cancer is relatively new, but the field is exploding quickly, according to Dr. Chen. In 2009, Hans Clevers, a researcher at the Hubrecht Institute in the Netherlands, first demonstrated that intestinal stem cells could form organoids. Dr. Clevers is a co-author on the Cell study, along with HOPP Chair Charles Sawyers, Genitourinary Oncology Service Chief Howard Scher, and many other members of MSK’s prostate cancer team.
Organoids derived from patient tumor samples, sometimes also called tumoroids, are being studied at Memorial Sloan Kettering and elsewhere for many other tumor types, including kidney, pancreas, and thyroid.
Watch a video of Dr. Chen discussing his research on Yahoo! News.