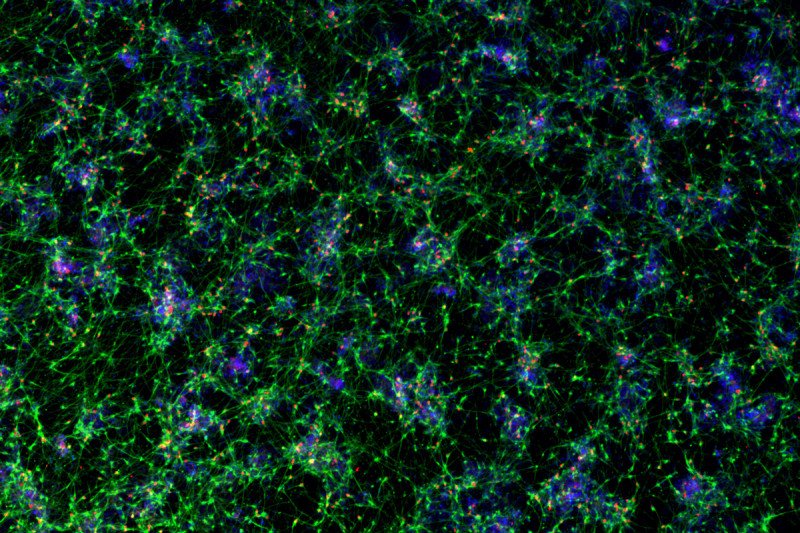
Growing neurons in a dish just got a lot easier. A new study from researchers at Memorial Sloan Kettering provides a quick and easy way to speed up development of cortical neurons, the cells making up the thinking parts of the brain. The improved method uses a combination of six molecules to, in effect, reduce the cells’ cooking time.
“Instead of waiting several months, we can make those neurons in about ten days,” says Lorenz Studer, Director of the Center for Stem Cell Biology at the Sloan Kettering Institute. “That’s a world record.”
The approach relies on what are called human pluripotent stem cells — versatile cells that can differentiate into any type of cell in the body. Such stem cells can be obtained from a developing embryo or produced by turning back the developmental clock of adult cells, in which case they are called induced pluripotent stem cells.
The ease and speed of the new procedure means that researchers can more readily model central nervous system diseases like schizophrenia and autism, and perhaps one day develop more-effective therapies.
A Neural Cookbook
The Studer lab had shown previously that they could use a similar method to create sensory neurons — specifically, ones that detect pain. That recipe, published in 2012, was useful but limited. Many of the diseases that strike the nervous system affect neurons in the brain rather than those in the peripheral nervous system (where sensory neurons are located).
The new approach provides a powerful tool to study these brain-centric diseases by producing the elusive cortical neuron. It relies on a combination of six molecules administered in a precise sequence and quantity to produce the desired product. The molecules are inhibitors of several molecular switches that are known to affect development, including WNT, Notch, FGF, and SMAD.
This formula, like previous ones from the Studer lab, was published in Nature Biotechnology.
Finding the Right Sequence
Contrary to the way some researchers screen for new drugs or biologically relevant molecules — testing thousands of different molecules in different combinations with machines, for example — the Studer team lit upon this particular recipe through a more artisanal approach.
“A theme of our lab is that we don’t use brute-force approaches to develop protocols,” says Yuchen Qi, a postdoctoral fellow in the Studer lab and the paper’s first author. “Instead, we focus on the real biological cues that we know to be involved in the development of these neurons.”
Still, it was tricky to come up with a winning formula. Much like baking a soufflé, the order in which you combine the ingredients, and how much you use of each, can make the difference between a successful pastry and a total flop.
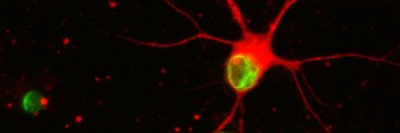
Cortical neurons growing in mouse brain
Switching metaphors, Dr. Studer likens the process to playing a piece of music. “There are only eight notes in an octave, but you can play those notes in many different ways,” he says. “It’s almost like each cell type has its own melody. Once you figure it out, you can get better and better at playing it.”
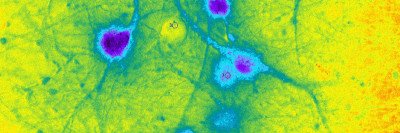
The music metaphor is appropriate given what the team did next: They implanted the human neurons in developing mouse brains and followed their growth using a powerful new visualization technique called iDISCO (which stands for immunolabeling-enabled three-dimensional imaging of solvent-cleared organs). With iDISCO, the team could create movies that show what happens to the human neurons over the course of six months as they boogied their way across the mouse brain.
“This shows that these cells can survive, and they behave like cortical neurons — going to the right places, for example,” Dr. Studer says.
Imagining the Future
Dr. Studer envisions a day when the neuron-growing method could be used to model a complex brain disease like autism or schizophrenia. “In the future, you could imagine being able to take skin cells from a schizophrenia patient, make induced pluripotent stem cells with them, then use this protocol to make cortical neurons,” he says. “Those neurons will have the same genetics — the same DNA — as the patient. You could then put these neurons in the mouse and ask, ‘How do they behave? Do they become wired up correctly? How are they different from normal neurons?’”
That may seem like a pipe dream, but it’s useful to remember that the Studer lab has a history of dreaming big and chasing down futuristic ideas. It was more than ten years ago that the team first learned how to create dopamine-secreting neurons from embryonic stem cells. They were able to show that these neurons can cure mice with a model of Parkinson’s disease, the devastating symptoms of which result partly from loss of dopamine-producing neurons in the brain. A clinical trial of these lab-created dopamine neurons for people with Parkinson’s disease is scheduled to open later this year, pending final approval by the Food and Drug Administration.