Recent findings by Memorial Sloan Kettering investigators suggest it might be possible to improve the effectiveness of chemotherapy for breast cancer by combining the treatment with a new type of drug called a cathepsin inhibitor.
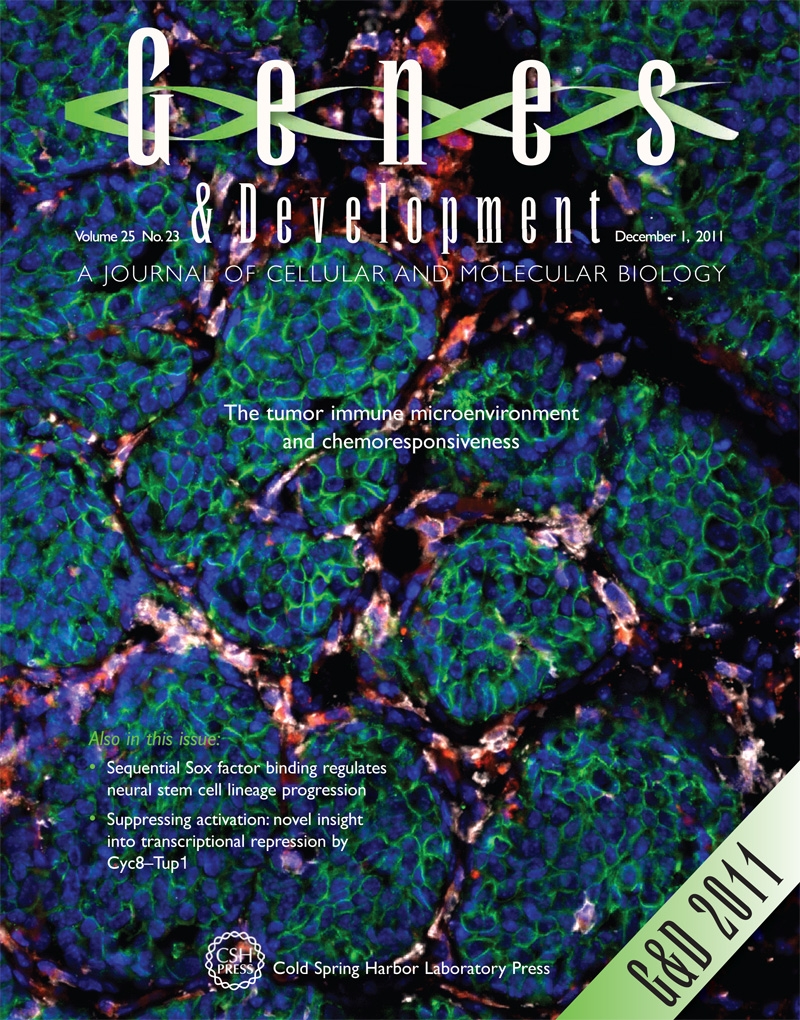
Working in mouse models of breast cancer and patient-derived breast cancer samples, the researchers have shed new light on how tumors interact with their microenvironment — the noncancerous cells, molecules, and blood vessels that surround a tumor — and the consequences such interactions might have for a cancer’s sensitivity to treatment. Their findings are published in the December issue of Genes & Development.
“Our earlier studies have shown that tumors are able to co-opt white blood cells called macrophages that exist in their environment, enticing these cells to secrete enzymes called cathepsins,” explains the study’s senior author Johanna Joyce, of the Sloan Kettering Institute’s Cancer Biology and Genetics Program.
Cathepsins secreted by macrophages play a role in a number of biological processes that enable tumors to grow and spread.
The researchers found that treatment with the chemotherapy drug paclitaxel (Taxol) can promote the infiltration of cathepsin-producing macrophages to tumors. The increased presence of macrophages results in tumor cells becoming resistant to several types of chemotherapy more easily.
“Our study is the first to show that macrophages are able to shield tumor cells from currently used chemotherapy drugs through a mechanism that depends on the activity of cathepsins,” Dr. Joyce says.
The researchers also found that breast tumors in mice responded better to paclitaxel treatment when the drug was delivered in combination with cathepsin inhibitors — investigational drugs designed to inhibit the activity of cathepsins — than when paclitaxel was given on its own.
“Our findings make a compelling case for the development of integrated breast cancer therapies — drug combinations that act simultaneously on tumors and their supporting microenvironment,” Dr. Joyce observes.

