Video: CAR T Cell Therapy: What It Is and How It Works
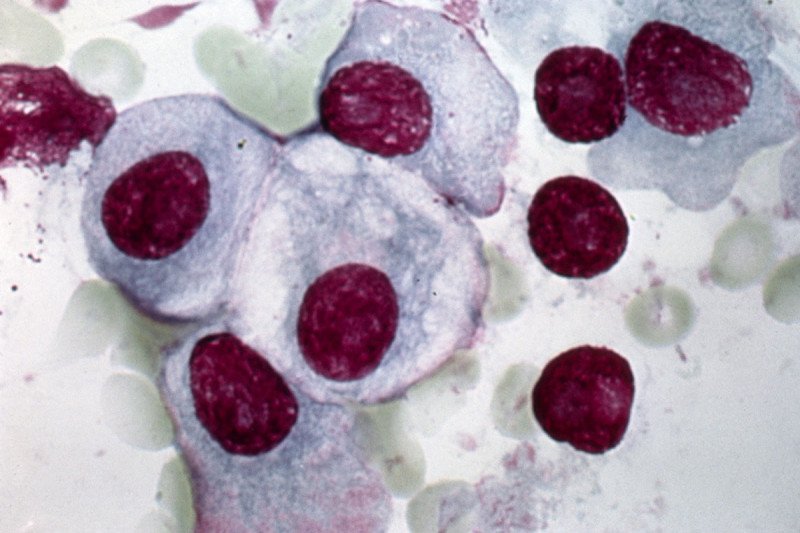
CAR T cell therapy, a type of cancer immunotherapy, is showing great promise for treating some patients with leukemia and lymphoma. In recent years, researchers have worked to extend this success to people with another blood cancer called multiple myeloma.
In order to work well, the CAR T cells need a good target on the multiple myeloma cells to recognize and home in on. One attractive candidate has been a protein called BCMA, which is found in abundance on multiple myeloma cells, yet absent from nearly all normal cells. Already, several academic institutions — including Memorial Sloan Kettering — are working with pharmaceutical companies to run clinical trials testing BCMA-directed CAR T cells in people with the disease.
However, many who receive this CAR T treatment have had their disease come back. There is evidence that people whose multiple myeloma cells have low or nonexistent BCMA levels are likely to experience relapse. To overcome this, scientists have been looking for an additional protein on multiple myeloma cells to take aim at.
A study led by MSK researchers suggests that the new target could be a receptor called GPRC5D. They found that, like BCMA, GPRC5D is present on the surface of multiple myeloma cells in most patients. The researchers also showed that CAR T cells engineered to lock in on GPRC5D were effective in mice with multiple myeloma.
The results are published in March 2019 in Science Translational Medicine. A clinical trial to test this approach in people with the disease could begin as early as summer 2019.
Pinpointing a Protein
MSK medical oncologist Eric Smith, who led the study, says that over the past seven years, several research teams at other institutions had reported that the GPRC5D gene was expressed in abnormally high levels in myeloma samples taken from patients. But none of those teams had been able to find the GPRC5D protein on the surface of the cells. The MSK-led team used a specialized staining technique to reveal the protein’s presence on the cell surface in abundance.
“We’ve shown that GPRC5D can be an attractive target for immunotherapy,” he explains. “It’s expressed on multiple myeloma cells and absent from nearly all healthy tissues, so there is less risk of side effects due to CAR T cells attacking normal cells.”
The CAR T cells that the MSK research team designed and tested are fully human, meaning they are free of mouse proteins that are sometime present in immunotherapies. This also reduces the chance that the person receiving the therapy will have a harmful immune reaction.
What’s Next: A Clinical Trial to Determine Safety
The upcoming phase I clinical trial will test GPRC5D-directed CAR T therapy in people with relapsed multiple myeloma. The trial will aim to determine if the new CAR T treatment is safe and to establish an optimal dose of cells to give.
If the trial establishes a dosage that is safe and effective, future trials would likely test GPRC5D CAR T cells in combination with CAR T therapy that targets BCMA, Dr. Smith explains.
“Unlike some CAR T treatments for leukemia and lymphoma, with multiple myeloma we don’t have evidence that we’re curing the patients with our current approach,” Dr. Smith says. “We know the disease is susceptible to CAR T therapy, but we haven’t found the exact recipe to generate lasting remissions and cures. Additional targets like GPRC5D may be the key to getting us there.”

