Cancer’s ability to spread throughout the body — a process known as metastasis — is responsible for the vast majority of cancer deaths. And a key feature of metastasis is that the cancer cells move, breaking away from a primary tumor and travelling to distant parts of the body.
Most of the time, however, the cells in our body stay put. So, to better understand how cells separate from a tissue, scientists at Memorial Sloan Kettering Cancer Center (MSK) focused their attention on one of the rare contexts when cells move around quite a bit: embryonic development.
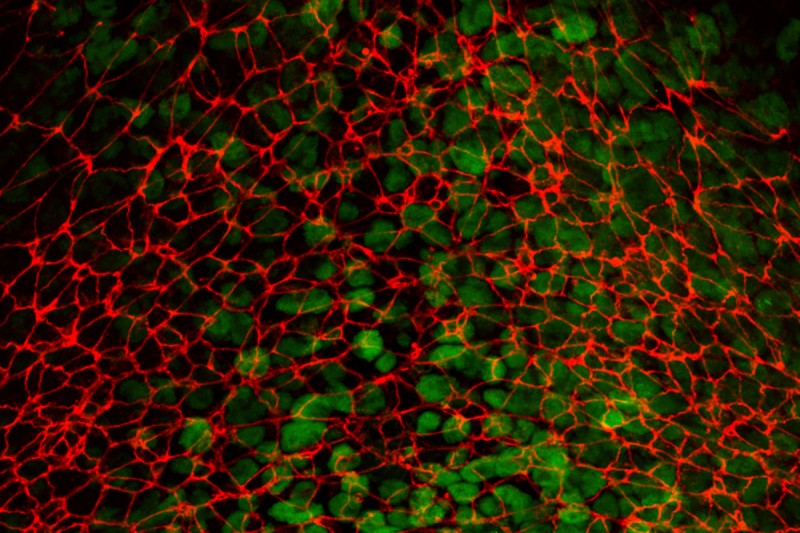
This new research from the lab of Anna-Katerina “Kat” Hadjantonakis, PhD, used high-resolution, time-lapse microscopy to better understand how developing cells break free from their tissue of origin during a process called epithelial-to-mesenchymal transition (EMT). Along with being a fundamental part of development, EMT is a hallmark of cancer metastasis, and studying the process in a developmental context can also help shed light on its role in cancer.
The study shows for the first time in detail how cells initiate this breakaway movement — capturing how they squeeze themselves out of a tissue by contracting their surfaces and changing their shape, along with identifying key proteins involved in the process. The findings were published May 10 in eLife.
“We know that cancer cells often hijack developmental programs to spread throughout the body,” says Dr. Hadjantonakis, Chair of the Developmental Biology Program at the Sloan Kettering Institute, a hub for foundational biology research within MSK. “That’s why it makes sense to have a developmental biology research program within a cancer center like MSK. Understanding precisely how these programs work in normal healthy cells can also tell us a lot about what happens in disease.”
Overcoming challenges to study cell movement during embryo development

For more than half a decade, senior research scientist Alexandre Francou, PhD, has been working on the puzzle of characterizing the behavior of cells as they break away from their neighbors in order to move throughout the embryo.
“This was quite a challenge. There were many technical hurdles to overcome,” says Dr. Francou, the first author of the eLife study. Before joining the Hadjantonakis Lab, he was a research fellow in the lab of study co-author Kathryn V. Anderson, PhD, former Chair of the Developmental Biology Program, who died in 2020.
Dr. Francou put EMT under the microscope, literally and figuratively. It’s a process during which epithelial cells, like the ones that line the internal and external surfaces of our bodies (think skin cells, but also the lining of our intestines and lungs) transform into mesenchymal cells (mobile cells that are important for building complex structures during development, and later for wound healing and tissue regeneration).
To turn into a more mobile version of themselves, epithelial cells have to lose some very important properties. This includes the ability to stick closely to their neighbors — which is really helpful for creating a continuous surface, like skin. Also, epithelial cells have a defined orientation (called polarity) so that the parts of the cell that interact with the world are on one side (the outward-facing side of the skin or nutrient-absorbing side of your intestine, for example), while the parts that anchor the cell to underlying tissue are on the opposite, inward-facing side.
The EMT the researchers were studying happens early in an embryo’s development during a process called gastrulation — that’s when cells originating in an epithelial layer break away and move around the embryo, to later form all the different organs and tissues.
The researchers created time-lapse movies of this EMT process in mouse embryos. This experimental mammalian model more closely resembles human development than simpler models like fruit fly and chicken embryos, which have been used in the past. But the mouse model came with its own challenges, Dr. Francou notes.
“In those other models, the cells undergoing EMT are at the surface of the embryos, and thus are directly accessible for imaging,” he says. “In the mouse model, these cells are internal, obscured by several layers of cells, and are difficult to access by microscopy. Additionally, the process also takes place as isolated events, as we think it happens in cancer metastasis, rather than all together across the tissue like in fruit fly models.”
So, Dr. Francou had to be persistent. He used genetically engineered mouse models in which fluorescent probes were attached to proteins-of-interest at the cell membrane. This allowed to visualize the surfaces of cells and their shape using high-resolution microscopy. And he combined this approach with sophisticated software to be able to analyze and quantify the changes in the cells.
“There’s a lot happening in these cells,” Dr. Francou says. “They’re constricting on one side, elongating on the other side, changing their shape, and detaching from their neighbors as they leave the tissue.”
Overall, the study shed new light on the molecular mechanisms underlying the EMT process in mammals. It found that to break away from their tissue of origin, cells contract in a series of ratchet-like pulses.
“You might think of it like tightening a belt buckle,” Dr. Hadjantonakis says. “These contractions happen in a similar type of step-wise fashion.”
And the study demonstrated that two groups of proteins important for preserving the architecture of cells are distributed unequally at their surfaces, and play critical roles in their contraction, which enables their escape from a tissue.
The researchers were also able to identify key similarities and differences in the process as it takes place in mammalian embryos, compared to invertebrate fruit fly embryo models.
How studying a developmental EMT can teach us about cancer metastasis

Studying developmental EMTs may offer new clues toward preventing cancer metastasis, the researchers note.
“The big idea is that understanding fundamental processes which normally occur during development as cells move around, and as organs and tissues are built, not only helps us understand the blueprints of life, but also gives us insight into disease and point towards new ways to attack cancer’s deadly progression to metastasis,” Dr. Hadjantonakis says.
“For example,” she adds, ”if we learn that specific proteins are necessary to help a cell break away from its neighbors before moving around the body and forming metastasis, then finding a way to block or disrupt those proteins locally could offer a potential strategy to prevent cancer cells from spreading.”
Dedicating the study to Dr. Anderson, her colleagues wrote: “Kathryn marveled at the spectacle of mammalian gastrulation, and recognized the insights that genetics and imaging would bring.”
This study was supported by the grants from the National Institute of Health (R01HD094868, R01DK127821, R01HD086478, and P30CA008748), and by a postdoctoral fellowship from the Alan and Sandra Gerry Metastasis and Tumor Ecosystems Center at MSK.