“The blueprint of life.” “The genetic code.”
The metaphors we used to describe DNA make it sound almost sacred.
Proteins, too, are revered. They are the “workhorses of the cell.” They make things happen.
RNA, by contrast, has not been so exalted. It is simply “the messenger,” a humble scribe relaying information from the nucleus, where DNA lives, to the cytoplasm, where proteins are made.
Transcription is the process of making a messenger RNA copy of a DNA sequence. It occurs in the cell nucleus.
Translation is the process of making a protein using the messenger RNA sequence in the cytoplasm. It occurs in the cell cytoplasm.
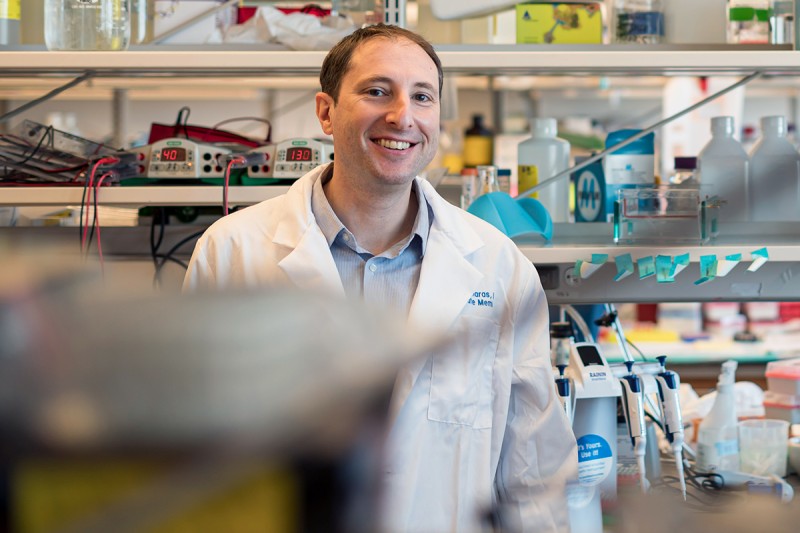
This popular textbook picture doesn’t tell the whole story, says Michael Kharas, PhD, a member of the Molecular Pharmacology Program in the Sloan Kettering Institute at Memorial Sloan Kettering Cancer Center (MSK), whose current work focuses on RNA biology, stem cells, and cancer.
“One of the quickest and most effective ways to change a cell’s fate is by altering which RNAs get translated into protein,” he says. “That makes RNA, and the proteins that bind to it, an attractive target for potential drugs to treat cancer.”
RNA as a Link Between Leukemia and Blood Stem Cells
While today Dr. Kharas is fascinated by RNA biology, he didn’t start his career being interested in it. That’s just where his scientific journey led him.
It began with his postdoctoral training at Harvard Medical School in the mid-2000s. Scientists were increasingly intrigued by a connection between cancer and stem cells — those perpetually youthful cells that divide repeatedly to replenish our tissues. His advisor and others had found that certain aggressive cancers appear to mimic the traits of stem cells — like being able to divide indefinitely.
Dr. Kharas was already familiar with one such aggressive cancer from his PhD work on leukemia, a type of blood cancer. That led him to wonder: might leukemia cells have something in common with the stem cells that make blood?
To answer that question, Dr. Kharas began comparing the genes that were active — that is, being transcribed and translated into protein — in both leukemia and blood-forming stem cells. He was looking specifically for proteins that were more abundant in both the stem cells and the cancer cells when compared with normal blood cells.
“That’s when we found Musashi,” he says.
Musashi: A Cell Fate Samurai
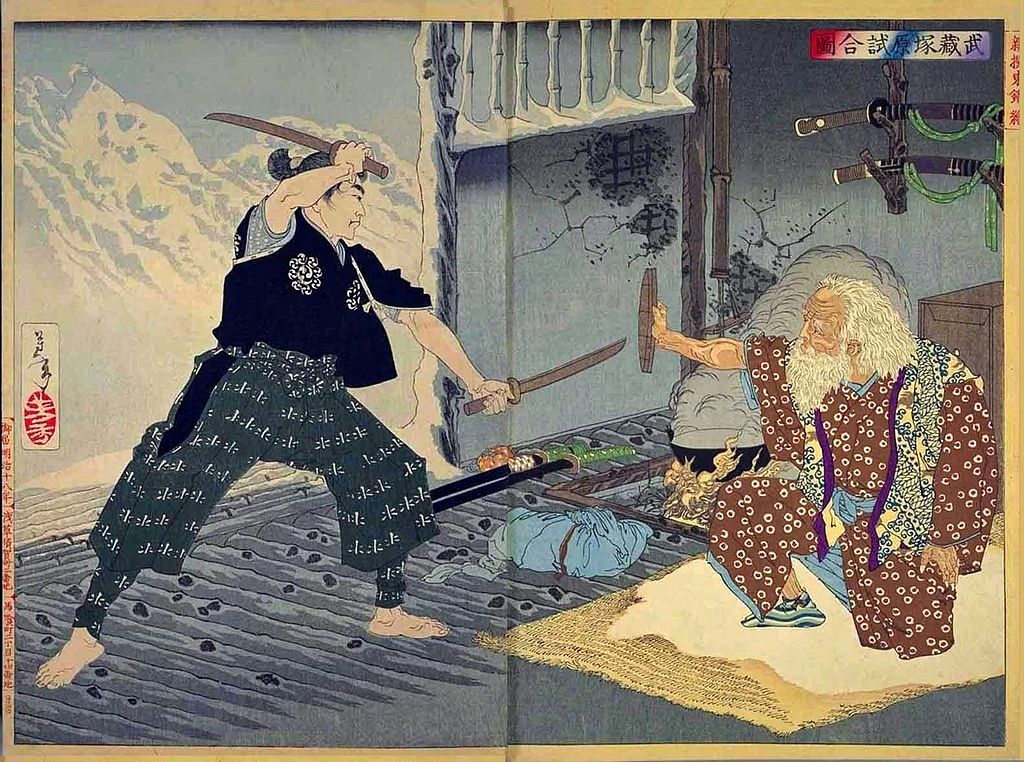
Musashi is a protein that binds to RNA. Like all RNA-binding proteins, Musashi’s role is to regulate what happens to the messenger RNA transcript once it’s been copied from DNA — for example, whether it is translated into protein, spliced into different forms, or degraded. The name Musashi comes from a mutant fly with two bristles instead of one and in that sense resembles the famous Japanese samurai who fought with two swords. (Fruit fly researchers have tended to name genes more colorfully than in other parts of science.)
When Dr. Kharas compared the two cell types, he found that both leukemia cells and blood-forming stem cells had lots and lots of the Musashi protein. That was the first clue that it was doing something important.
To find out what exactly it was doing, Dr. Kharas and his colleagues performed additional experiments to ask what would happen if they changed the amount of the Musashi protein present in the two types of cells.
The results were dramatic: lowering the amount of Musashi in blood stem cells reduced their ability to make new blood cells, while raising the amount of Musashi in blood stem cells led to an aggressive leukemia.
In leukemia cells, lowering the amount of Musashi led to decreased cell growth and division, while raising it made the cancer cells more aggressive.
What’s more, the results of these laboratory experiments mirrored what was happening in patients. The amount of Musashi present in leukemia cells from patients correlated with patient survival. The more Musashi, the worse the survival.
Dr. Kharas’s conclusion was that Musashi is part of the normal process that determines the fate of a blood-forming stem cell — instructing it to either remain a stem cell or to start differentiating into a blood cell. He also concluded that leukemia cells rely on Musashi to become more like stem cells and therefore more aggressive.
And how was Musashi was doing all this? Simply by regulating which RNAs get translated into proteins and which do not.
Potential Drugs to Halt Leukemia Progression
These days, people are much more aware of the power of manipulating RNA for therapeutic effect. The COVID vaccines were based on RNA, for example. But back when Dr. Kharas got hooked on RNA biology, scientists were just starting to become interested in it.
“This was a space that at that time was just really emerging,” he says. “It’s really exploded in the last few years.”
Since his initial discovery of Musashi’s role in leukemia, he’s been exploring the network of processes that Musashi is a part of. It’s been an especially rich vein to mine.
Targeting IKZF2 and CK1α Proteins To Treat Leukemia in Mice
Most recently, he and his team collaborated with researchers at Harvard to develop drugs that can degrade one of Musashi’s main accomplices, IKZF2, and another leukemia-associated protein called CK1a. These proteins are necessary for leukemia progression, and degrading them with drugs can arrest leukemia progression in laboratory mice. The drugs aren’t yet approved for use in people, but the team is working to develop versions that might one day be used in the clinic.
Targeting RNA methylation in cancer
They’ve also been exploring the wider world of RNA biology, unrelated to Musashi.
Along with Samie Jaffrey, MD, PhD at Weill Cornell Medicine, Dr. Kharas and his team were among the first to show that RNA methylation is important in cancer. Methylation is the process whereby cells add small molecules, called methyl groups, to other molecules. Like DNA methylation, RNA methylation is a powerful way to control what genes get translated into proteins. Dr. Kharas found that the machinery that methylates RNAs is ramped up in leukemia. Drugs that target the RNA methylation machinery in cancer cells are now in phase 1 clinical trials.
MSK’s Leadership in RNA Biology Research
Kharas credits MSK with providing the kind of collaborative and supportive environment necessary for scientists to conduct world-class research.
“Everyone here is mission-driven and curious,” Dr. Kharas says. “The competition we feel isn’t with each other. It’s more about competing with the world, trying to drive the important scientific questions as leaders in the field. People look to us to be the role models of doing science in the best possible way.”
As for Musashi, there is still plenty to learn, Kharas says, but he expects that new technologies coming down the pike will allow them to take RNA biology to the next level.
He adds: “It’s been an adventure and I’m excited to see what happens next.”