When Chris Scott met with his urologist in January 2022, he thought they’d talk about an issue he was having with his prostate. But the conversation took a very different turn after Chris, 61, got a CT scan of his abdomen. On his pancreas was a cyst the size of a grape. The urologist referred Chris to a gastroenterologist, who ordered a biopsy. The results were shocking: If left untreated, the cyst was likely to morph into an aggressive form of pancreatic cancer.
Chris reached out to pancreatic cancer surgeon Alice Wei, MD, who specializes in Whipple procedures at Memorial Sloan Kettering Cancer Center (MSK). A Whipple procedure is a complex operation to remove parts of the pancreas and small intestine, as well as all of the gallbladder and bile duct. Cancers in these organs, which make up the digestive system, are often grouped together as hepatobiliary (HPB) cancers.
After reviewing his scans, Dr. Wei determined that she could offer Chris a minimally invasive surgery called a robotic Whipple. It could both prevent cancer and give him an excellent quality of life. Chris didn’t hesitate.
“I was all for moving forward,” says the New Jersey real estate agent. “I was a ticking time bomb. I was confident in my meetings with Dr. Wei.”
He also trusted MSK’s expertise. “Only 3% of hospitals nationwide do 20 open Whipples every year,” Dr. Wei says. “We are doing that many robotically.”
Traditional Versus Robotic Whipple Procedure
More than 90% of Whipple procedures are traditional open surgeries. Open surgery is what most people imagine when they think of surgery — making a single incision so that the surgeon has a full view of the organs. A traditional Whipple procedure can take up to 12 hours and require a week of recovery in the hospital.
Robotic surgery is much different. The surgeon sits at a console and uses hand and foot controls to guide their surgical instruments, which are held by a mechanical arm. The console’s high-definition cameras project a three-dimensional image that can be magnified as much as 10 times. This dramatically enlarged image enables the surgeon to make much smaller incisions.
The robot is also more sensitive to the slightest movements of the surgeon’s wrist, hand, and fingers, which increases the surgeon’s precision.
A robotic Whipple procedure requires only six small incisions, about the size of a keyhole, which result in less blood loss. The operation can take just eight hours and shorten hospitalization to four to five days. There’s better pain control and minimal scarring, too.
Dr. Wei says to understand the difference between the two surgeries, think Google Maps. “Open surgery provides a satellite view, and robotic surgery is more like a street-level view,” she says.
Who Can Get a Robotic Whipple Procedure?
Dr. Wei notes that right now, the robotic Whipple is meant for patients who have not had a related abdominal surgery and whose tumors are not connected to blood vessels. Today, about 10% to 15% of robotic Whipples are done for precancerous tumors like Chris’.
But the eligibility criteria are expanding, and Dr. Wei hopes that in 5 to 10 years, the robotic Whipple will become a mainstay of cancer surgery.
“We’re seeing amazing results,” Dr. Wei says. “And we want to build on that.”
Pioneering the Robotic Whipple Procedure at MSK
Dr. Wei founded MSK’s robotic Whipple program in 2020. In just two years, she has performed more than 30 procedures. International guidelines consider 20 to be a high volume.
“It’s meeting a very high bar,” Dr. Wei says.
MSK had already been using robotic surgery for patients with colorectal, prostate, uterine (endometrial), and other cancers. HPB cancers were “the final frontier in robotics,” Dr. Wei says. “The reason we wanted to start this program is because it’s the future.”
Chris’ Quick Recovery From the Robotic Whipple
Chris had his robotic Whipple on August 8. He had a minor abdominal blockage over Labor Day weekend, which improved over a couple of days with rest and rehydration.
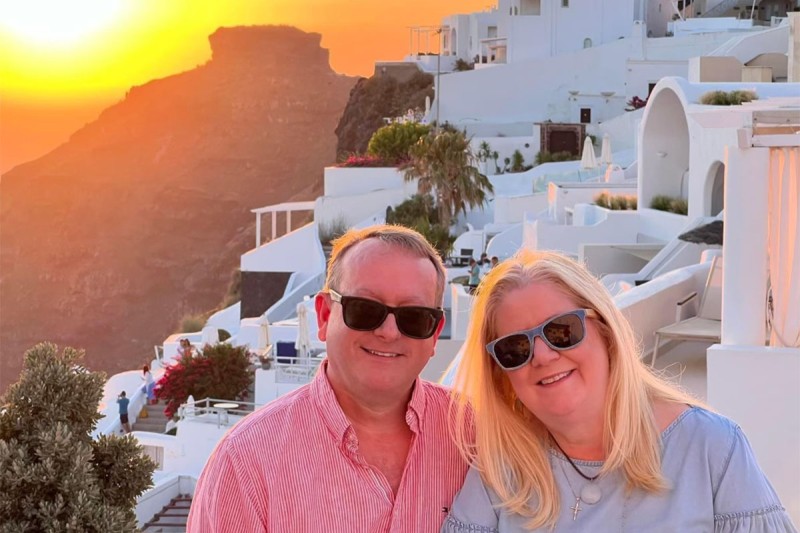
Chris recuperated so quickly that he, his wife, and a group of friends took a trip to France one month after the surgery.
“We had planned it a year ago, and I felt well enough to go,” he says. He toured villages, went hiking, and enjoyed wine tastings. “It was a real confidence booster,” he adds.
Dr. Wei says Chris’ trip demonstrates the real-life benefits of the robotic Whipple.
“To travel abroad after surgery — you can’t measure that,” Dr. Wei says. “We have made great strides in the science of surgery so that it is much less disruptive. MSK surgeons do these specialized operations day in and day out. The more often a surgeon does a procedure, the more skilled they are at ensuring patients have a smooth recovery and maintain an excellent quality of life.”