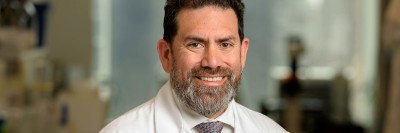
Luis Diaz, Jr., Head of the Division of Solid Tumor Oncology at Memorial Sloan Kettering.
Two years ago at the annual meeting of the American Society of Clinical Oncology, researchers from Johns Hopkins wowed an audience with results from a recent immunotherapy clinical trial. People with a type of colorectal cancer that bore a genetic abnormality called mismatch repair (MMR) deficiency fared surprisingly well when treated with the immunotherapy drug pembrolizumab (Keytruda®). In fact, 62% of them responded to the treatment.
The result was remarkable because colorectal cancer patients typically do not benefit from this type of immunotherapy, called an immune checkpoint inhibitor. None of the other colorectal cancer patients in the study responded at all.
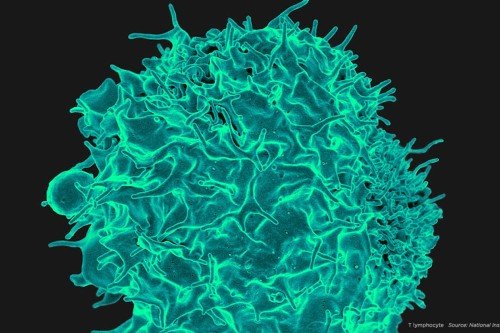
Experts celebrated the findings as bolstering an emerging concept in the field of immuno-oncology, that the more DNA mutations a cancer cell has, the higher the likelihood it will be recognized by the immune system as foreign and killed.
MMR-deficient cells have lots of mutations — 1,700 on average compared with just 70 in a typical cancer cell. That’s because the mismatch repair pathway is a major way that cells fix DNA base-pair mistakes that occur during DNA replication, which cells must do each time they divide.
The Hopkins-led trial eventually enrolled people with a dozen different cancer types that all shared this genetic defect. Together, the results showed that the potential for an excellent response to immunotherapy was not unique to MMR-deficient colorectal cancer. It held true for all of the MMR-deficient cancers, regardless of their tissue origin.
These striking results served as the basis for the Food and Drug Administration’s approval of pembrolizumab for advanced MMR-deficient cancers last month. This was a landmark event in oncology. It represents the first time that a drug has been approved on the basis of a specific genetic profile rather than where the cancer originated.
“It’s a shift in how we develop anti-cancer therapeutics,” says Luis Diaz, Jr., a medical oncologist at Memorial Sloan Kettering. Dr. Diaz was the principal investigator on this trial when he was a professor of medicine at Johns Hopkins. He recently moved from Hopkins to Memorial Sloan Kettering to assume a new role here as Head of the Division of Solid Tumor Oncology.
“It’s not only a pan-tumor approval for adult tumors, it also includes pediatric tumors. So it’s agnostic to both age and tumor type,” he says.
Science Behind the Study
In a new paper published in Science, Dr. Diaz and his colleagues report in detail on the results of the clinical trial. Among the 86 people in the trial, there were 12 different types of cancer. More than half of the participants (46 patients) had an objective response to pembrolizumab, a PD-1-blocking drug. That means their disease became smaller. Of these 46, 21% (18 patients) had a complete response, meaning the cancer vanished. The disease control rate, or the percentage of people whose disease either remained stable or improved, was 77% (66 patients). Responses were often durable.
These are impressive results for a cancer clinical trial, and even more impressive for an immunotherapy trial. Typically, a smaller fraction of people responds to a single-drug immunotherapy.
In fact, the number of people who had a complete response is probably higher than reported. This is because what looks like cancer on an imaging scan might actually be the battle scars left after the immune system has done its work.
“We biopsied patients at 20 weeks who appeared to have residual disease on their scans. What we found was that the majority of these ‘tumors’ were just scar tissue,” Dr. Diaz explains.
In addition to reporting on the trial’s results, Dr. Diaz and colleagues delve into the underlying cause of immune responses to MMR-deficient cancers. For three patients who had a good response to pembrolizumab, the team analyzed the genetic attributes of both the tumor tissue (which had been removed prior to treatment and archived) and the immune cells circulating in the blood. They found that T cells specific for particular neoantigens — the fragments of altered proteins produced from mutated DNA — were present in the tumor before treatment, and these cells rapidly and dramatically increased in the blood following treatment.
As the authors note, these results support the hypothesis that the large number of neoantigens present in MMR-deficient tumors makes them responsive to immune checkpoint blockade therapy. This approach is often likened to releasing the brakes on immune cells, allowing them to attack cancer. Side effects of these drugs can include autoimmune reactions, caused when the immune system attacks normal tissues in the body.
A Telling Observation
Dr. Diaz notes that the inspiration for the MMR study goes back to a clinical trial that his Hopkins colleagues Suzanne Topalian and Drew Pardoll conducted. The results of that study were published in 2012. In the trial, a single colorectal cancer patient had a dramatic response to the PD-1-blocking drug nivolumab (Opdivo®). The patient was subsequently found to have Lynch syndrome, an inherited form of mismatch repair deficiency. Dr. Diaz surmised that the high mutational burden in this patient made the cancer more recognizable to his immune system.
“So then it was off to the races,” Dr. Diaz says. “I knew we had to conduct a trial.”
They did, and based on the trial’s early results, the FDA granted the approach a Breakthrough Therapy designation in October 2015. Final approval of pembrolizumab for MMR-deficient tumors came in May 2017.
Dr. Diaz notes that the trial never would have happened without the groundbreaking work of many researchers, including several at MSK, who established the promise of immunotherapy as a cancer treatment. “Jedd Wolchok and his colleagues really helped define that immune checkpoint inhibitors could be a potent class of anticancer drugs,” Dr. Diaz says. “We wouldn’t be here today without his work.”
Around the same time that Dr. Diaz and his group were conducting their study, Dr. Wolchok and MSK researchers Timothy Chan and Alexandra Snyder Charen showed that mutational burden was an important variable influencing immunotherapy responses in lung cancer and melanoma.
And in 2008, it was work by immunologist James Allison (then at MSK) and MSK physician-scientist Neil Segal, in collaboration with cancer biologist Bert Vogelstein at Hopkins, that established mutant proteins could create neoantigens recognizable by the immune system.
A Big Impact
Dr. Diaz notes that about 60,000 people a year will be eligible for this immunotherapy on the basis on their mutation profile. He estimates that about 4% of all cancers are likely to be MMR deficient.
Witnessing the dramatic effect of immunotherapy on people with MMR-deficient tumors who had otherwise run out of options has made him optimistic about the power of this approach to make a profound difference in people’s lives. He notes that a couple of the patients were in hospice when they enrolled in the study and are still alive today.
“I feel lucky to be a part of this breakthrough,” he says.