
Armani Rodriguez was only 2 months old when he spent his very first Christmas in a hospital. Now 22 years old, the Brooklyn native can’t recall the searing pain that landed him there, but his mom will never forget.
“He was always crying and needing pain medication,” says Awilda, Armani’s mother. She remembers a heart-wrenching cycle of emergency room visits, hospital stays, and procedures, but the pain would always come back.
Armani was born with sickle cell disease (SCD) — an inherited blood disorder in which red cells become crescent-shaped, fragile, and inflexible, and don’t flow normally in the blood. They get stuck in tiny blood vessels and restrict blood and oxygen flow. This often leads to sudden episodes of extreme pain known as a crisis. In addition to anemia, SCD can also cause other serious health issues including stroke, organ damage, and acute chest syndrome (a severe lung-related complication).
“Symptoms usually start in infancy, and problems with pain and other complications get worse over time,” says Maria Cancio, MD, a hematologist-oncologist at Memorial Sloan Kettering Cancer Center (MSK). She cares for children and young adults with life-threatening blood disorders at MSK Kids.
His First Bone Marrow Transplant for Sickle Cell
After years of countless hospital visits and treatments, Armani had a bone marrow transplant (BMT) at another hospital when he was 8 years old. This procedure replaces blood-forming stem cells with new healthy ones. For the best results, a relative who is a good genetic match is needed to donate their stem cells.
Luckily, Armani’s older brother, Brian, was a perfect match, and he was able to donate his healthy stem cells. The transplant seemed to work. Armani and his family thought he was finally free of the disorder that had caused so much pain and heartache.
After an SCD Relapse, Hope at MSK
Sadly, signs of SCD came back 12 years later. “I felt excruciating pain, and it was bad. I couldn’t even breathe. The worst pain was in my back,” says Armani, who was suffering from vertebral collapse, a common complication of SCD. His bloodwork showed that Brian’s donor cells were slowly disappearing, and the sickle cell levels were rising. At age 20, Armani had relapsed.
“The terrible pain made him walk like an old person. He couldn’t get out of bed,” remembers Awilda. “It was really hard for him to go through this as a young adult because he forgot how bad the pain was when he was little.”
A family member recommended that Awilda request a consultation at MSK to discuss the next steps in Armani’s care. They were set up with Dr. Cancio, who immediately put Armani and his mother at ease. “Dr. Cancio is like family. She treats me so nice and is always cheery and supports me no matter what,” says Armani. “She gave me hope.”
Awilda agrees. “Dr. Cancio made me feel calm and confident that Armani was going to be OK,” she says.
Feeling Supported Through Shared Culture and Language
Sickle cell disease is most common in people of African American and Hispanic/Latino descent. Of the estimated 100,000 people affected by SCD in the United States, about 10,000 of them live in New York.
MSK reflects the diversity of nationalities and ethnicities in New York and throughout the world. MSK Kids sees patients from nearly 70 countries and its staff speaks more than 25 languages. Many MSK physicians like Dr. Cancio are bilingual and can communicate with patients in their preferred language.
“Armani and his mom are fully fluent in English and Spanish, but it’s nice to have that special connection with someone who understands your culture and is part of your village,” says Dr. Cancio, who is of Puerto Rican descent. In fact, more than a quarter of the families admitted to the Pediatric Stem Cell Transplantation and Cellular Therapies (TCT) Service at MSK Kids speak Spanish.
Awilda felt a connection right away. “When I first met Dr. Cancio, it was like I knew her from before. We are both Latina and got along well,” she recalls. “She communicated with Armani using simple words he could understand. She spoke with him in English and Spanish so he could feel more comfortable.”

Dr. Cancio also provided extra care as she guided them through the difficult transplant and recovery process. “We don’t routinely Facetime with parents of adult patients during clinic visits, but I did whenever possible as a special gesture and added layer of support for Armani’s family, and they appreciated it,” says Dr. Cancio.
Personalized Treatment for Sickle Cell Disease
Dr. Cancio explained that Armani would need another BMT. He would first receive a new combination of stronger, more effective chemotherapies than he had before. The regimen eliminates the sickle cells and prepares the bone marrow to receive the transplanted donor cells.
“It’s like putting a nuclear bomb in the bone marrow,” says Dr. Cancio. “You’re wiping out every damaged cell in the bone marrow to reduce the chance of having a mixed ratio of sickle cells and donor cells. We want 100 percent donor cells.” She was also able to customize the dose of some of the chemotherapies for Armani’s metabolism, size, weight, and other factors to help minimize the risk of complications.
“That chemotherapy was tough, but he came through it like a champion!” says Awilda.
Once again, his big brother generously donated his stem cells. “Brian is a hero,” says their mother, “We are blessed to have him.”
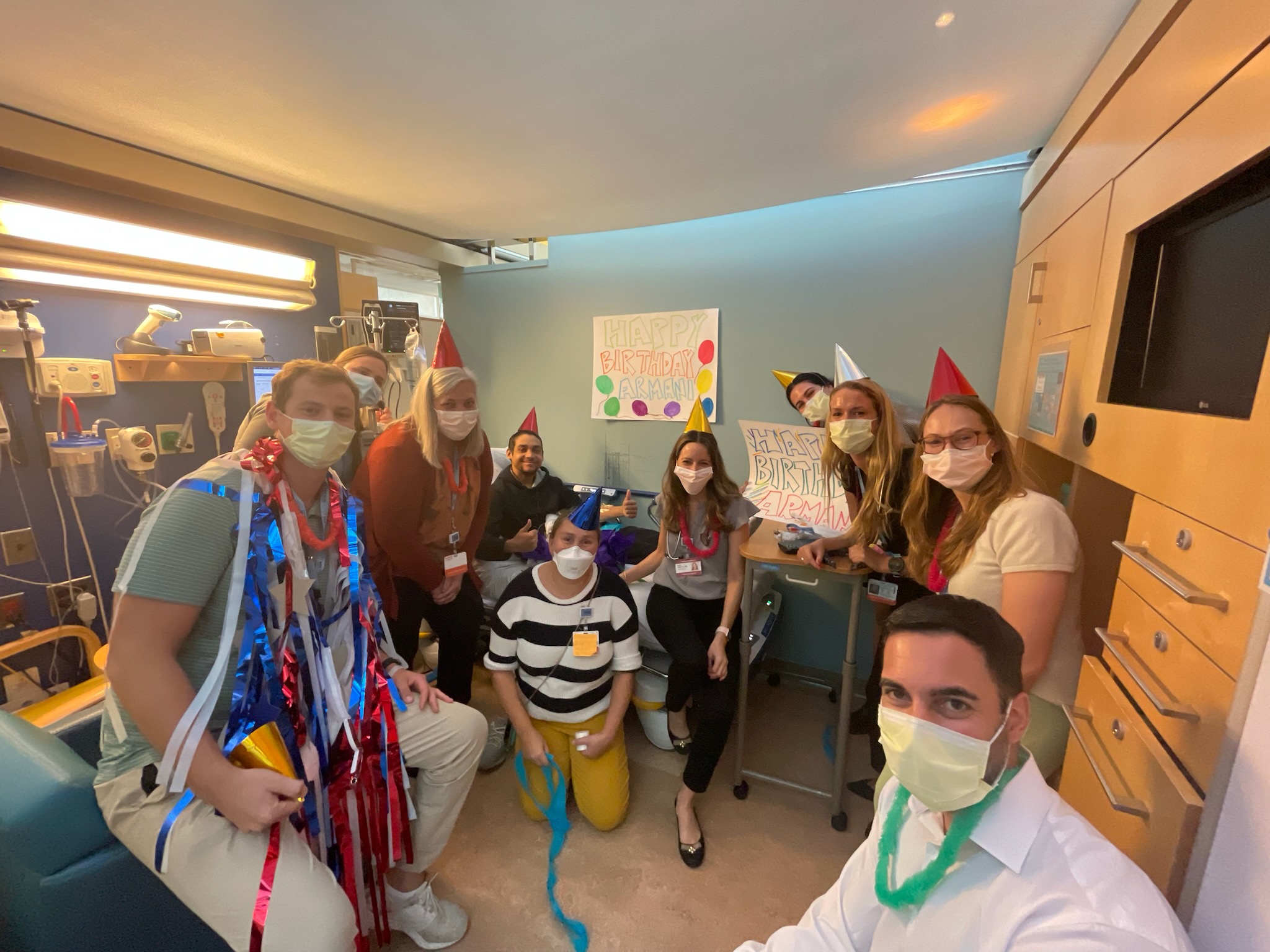
Armani spent two months in the hospital during the BMT process. “The whole MSK team was great. The nurses made everything go so smoothly,” says Awilda, who says they made Armani feel at home. To celebrate his 21st birthday, they decorated signs, donned party hats, and gathered in his hospital room.
Feeling Normal Again After SCD Cure
Two years after the BMT, Dr. Cancio says that Armani’s bloodwork shows no sickle cell disease; he is effectively cured. He has no pain, no long-term complications, and comes in to MSK just once a year for a checkup. “He’s a really sweet boy and it’s so good to see him healthy now,” she says.
Armani is now enjoying his new job working at a summer camp with middle school children. “I feel amazing!” says Armani. “I wake up every day feeling normal. I’m pain-free!”
Gene Therapy for Sickle Cell Disease: MSK at the Forefront
Although the survival rate and quality of life for people with SCD has improved thanks to new medications, an entirely new approach — called gene therapy — holds promise as a more targeted and effective treatment. In December 2023, the U.S. Food and Drug Administration (FDA) approved the first cell-based gene therapies for people 12 years and older.
MSK Kids is the first hospital in the New York City region to offer one of these therapies, known as Casgevy®. It’s the first approved treatment to modify a patient’s own blood stem cells using a type of new genome editing technology called CRISPR, which is revolutionizing research and medicine. Stem cells are removed from the body, and the sickle gene is changed or edited to help restore the cells’ ability to make healthy red blood cells. The treated stem cells are then infused back into the patient.
A major benefit of gene therapy is that the patient is their own cell donor. “Not having to find a donor is a huge advantage because patients with SCD don’t always have a sibling who is perfectly matched and healthy enough to donate their cells,” says Dr. Cancio, who studies gene therapy in clinical trials for people with SCD. “And African Americans and Hispanics are less represented in the bone marrow registry, so it’s harder to find an unrelated matched donor.”
Using one’s own cells also eliminates the risk of graft versus host disease, a BMT complication that happens when the donor’s immune cells attack the recipient’s tissues.
Dr. Cancio says families must consider all the pros and cons of gene therapy. For example, as with a BMT, gene therapy requires high-dose chemotherapy, and the process involves a lot of time in the hospital. The long-term effects of these brand-new therapies are not yet known and will continue to be studied.
“These treatments are also very expensive, not covered by all insurance companies, and they are only done at a handful of centers in the world, so there is limited availability for patients,” explains Dr. Cancio. “However, because they drastically reduce or eliminate pain, they can transform patients’ lives in a positive way and open up new therapeutic avenues for people with SCD.”
Meanwhile Armani is thriving, and his mother says she is grateful for the excellent care he received at MSK.
“My son is no longer in pain and has a future,” says Awilda. “And Dr. Cancio has become like family to us.”
