For some people with cancer, immunotherapy drugs called checkpoint inhibitors, which take the brakes off the immune system and allow it to attack cancer cells, have been a game changer. They can shrink even very advanced cancers to levels that can no longer be detected. But for most patients, these drugs have been disappointing. Researchers are trying to figure out why.
Now the largest-ever genetic analysis of people being treated with checkpoint inhibitors has found that certain genes people are born with (called germline genes) may play a critical role. We spoke to Memorial Sloan Kettering physician-scientist Timothy Chan, one of the study’s senior authors, about what his team found and what their findings may mean for people with cancer.
How is this study different from other studies looking at response to immunotherapy?
First, it was very large. We looked at more than 1,500 people who were treated with checkpoint inhibitors for a number of cancers. Our study included people across many different types of cancers. This leads us to believe that what we found applies very broadly, and not just to people with one type of cancer being treated with one particular drug.
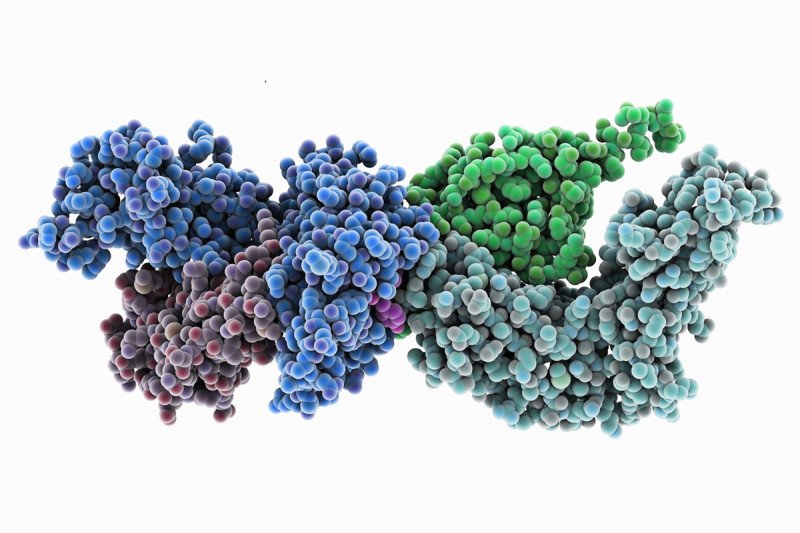
Another difference is that we looked not only at genetic changes inside the tumor tissue, which many other studies have done, but also at certain genes that people are born with. Those genes make up people’s normal DNA. Specifically, we looked at human leukocyte antigen (HLA) genes. These genes are critical for regulating the immune system and dictating what it can detect and fight off.
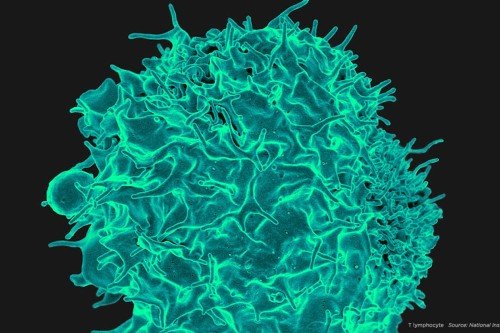
Importantly, the HLA system is used to match recipients and donors for stem cell and bone marrow transplants. HLA genes guide immune cells called T cells to recognize what is “self” and what is not. For transplants, we want the donor’s HLA system to be similar enough to the recipient’s that donated T cells will not attack the recipient’s tissues. In the case of cancer, we want to boost the T cells’ ability to destroy tumor cells, and HLA proteins determine what T cells can see. No previous study has closely examined the effects of HLA germline genes on immunotherapy response.
What gave you the idea to look at these HLA genes and how they relate to immunotherapy response?
Researchers have known for a while that HLA genes play a role in how people respond to infections. Certain HLA profiles are associated with better outcomes in people with HIV, hepatitis B, and malaria. HLA genes are among the most diverse of all human genes. Our species has evolved such diversity to improve the ability of our immune system to overcome infections. For example, in Africa, where malaria is common, people have evolved HLA genes that help them recognize and fight off those particular infections. In other areas of the world, people may have evolved HLAs to fight off infections that are common there. The human body is constantly under assault from pathogens, and HLAs are how we recognize and eliminate them.
We wanted to see how HLA genes in patients affect their response to anticancer immunotherapy.
What was different in the HLA genes of people who responded to checkpoint inhibitors compared with those who didn’t?
We found in our study that people who had a greater diversity and more variation in their HLA genes responded much better to immunotherapy compared with those who had less diversity. Because no one had ever before looked at HLA genes in people undergoing immunotherapy, this was a new finding.
Did this finding surprise you?
Not completely. Several years ago, our group at MSK and investigators elsewhere began looking at the effects of the tumor genome on immunotherapy response. We found that tumors with a greater number of mutations were more recognizable to the immune system.
Our latest findings represent the other side of the same coin: Just as tumors with a greater number of genetic changes are more recognizable to immune cells, having more-diverse HLA genes means that someone’s immune system has a greater ability to recognize what doesn’t belong inside the body. Both are important for maximizing the ability of the immune system to see and destroy cancer cells.
As more people around the world are being treated with checkpoint inhibitors, it was observed that different response rates occurred in different parts of the world. For example, studies conducted in northern Europe have shown that overall a lower percentage of people respond to some of these drugs. This makes sense in light of our new findings, because those populations are known to have less diversity in their HLA genes.
Will this finding change how patients are treated?
I think it will have a strong effect very soon. There is a rush to develop genetic tests to measure how many mutations are present in tumors as a way to predict response to immunotherapy. We have shown that someone’s DNA — their HLA genes — is critical as well. We can combine information about HLA diversity with data on numbers of mutations to make much better prediction models for checkpoint inhibitor response.
For instance, in people who have a low diversity in their HLA genes as well as a low number of mutations in their tumors, we know they are much less likely to respond to checkpoint drugs, especially when those drugs are given alone. So we may want to treat them with a combination of different immunotherapy drugs instead of just one, or try targeted therapies or other treatments instead.
The MSK-IMPACTTM test, which recently received authorization from the US Food and Drug Administration, already analyzes the HLA genes in patients’ blood samples. So at MSK we can start using these new findings right away. Other tests that look at tumor genomes don’t include HLA analysis. This is one more component that illustrates the power of MSK-IMPACT and what makes it unique.
What are the next steps for this research?
Our findings will need to be validated in prospective studies, but because we included such a large and diverse number of patients — more than a thousand — we think we’ve set the bar pretty high.
We can’t do anything about the HLA genes that people are born with. But we think that learning more about immune system recognition can help with the development of new cancer treatments, such as vaccines that could be used on their own or in combination with checkpoint inhibitors. The differences in how various HLA genes work to promote tumor rejection can help guide the choice of targets to use in new anticancer vaccines.