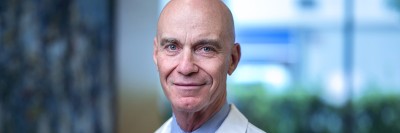
Clinical geneticist Kenneth Offit (left), shown here with genetic counselor Yelena Kemel, is leading a study on BRCA testing.
In March 2018, the US Food and Drug Administration approved an at-home, mail-in kit that tests for some of the inherited mutations in the genes BRCA1 and BRCA2. These mutations are linked to an increased risk of breast cancer, ovarian cancer, and prostate cancer, and possibly others.
Storefront centers that conduct cholesterol checks, do thyroid panels, and screen for sexually transmitted diseases have made people more comfortable initiating their own medical tests. But many experts say that some types of testing — including for cancer genes — should continue to be done under a healthcare provider’s guidance.
“The developers of at-home genetic tests have said they should be as easy and available as a pregnancy test, which any woman can take at home alone in her bathroom,” says Kenneth Offit, Chief of MSK’s Clinical Genetics Service. “But that’s exactly what we’re worried about. For men and women, finding out that you’ve inherited a cancer gene can raise a lot of issues. We want to make sure that people who receive these results are getting the support that they need.”
To answer some of the questions about the best way for people to get this kind of health information, a team of clinical genetics experts has launched the BRCA Founder Outreach (BFOR) study. The study is being led by Memorial Sloan Kettering and three other cancer centers.
A Contrast to Recreational Genomics
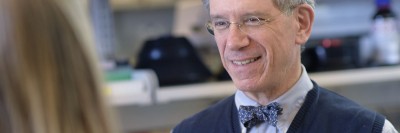
“Thanks to new avenues of communication and education, we can enhance genetic counseling and widely share the knowledge of top experts when screening for cancer genes,” explains Mark Robson, Chief of the Breast Medicine Service and a co-principal investigator of the study. “BFOR is designed to help us do that.”
The purpose of the BFOR study is to evaluate how to best combine the convenience of direct-to-consumer genetic tests with guidance from a medical care provider. It will allow 4,000 women and men with Jewish ancestry to enroll in screening for the three most common BRCA mutations linked to increased cancer risk. These mutations are quite rare in the general population, but one in 40 people of Ashkenazi (Eastern European) Jewish descent carries at least one of them.
“This is not recreational genomics, which is what most home-testing kits have traditionally been,” says Dr. Offit, who is one of the principal investigators and head of the executive committee running the BFOR study. “The stakes for these kinds of cancer genetic tests are much higher than just looking at your ancestry.”
People who are age 25 and older and have one or more Ashkenazi Jewish grandparent can go to the BFOR website and fill out a questionnaire to determine whether they are eligible. Once they complete the online educational and consent process, they can go to a local Quest Diagnostics center to get a blood test. Quest is providing testing at no charge to the study participants.
Explaining Potentially Life-Changing Genetic Test Results
Under the BFOR model, participants receive the results from someone who can explain what the findings mean, rather than getting them in the mail. They can choose whether to get their results from a clinical genetics expert or their own doctor. Some of the issues raised by learning of an increased cancer risk include whether to consider risk-reducing surgery and how to inform other family members who may also carry the mutation.
Currently, the study is limited to people living in metropolitan areas that have participating centers, so they have access to genetics experts. In addition to MSK in New York City, the other sites involved are Dana-Farber Cancer Institute and Beth Israel Deaconess Medical Center in Boston, the University of Pennsylvania in Philadelphia, and Cedars-Sinai Medical Center in Los Angeles.
Another important note is that with both the BFOR study and the commercial genetic-testing service, only the three most common BRCA mutations are included. These three mutations account for about 95% of BRCA1 and BRCA2 mutations in Ashkenazi Jews. BRCA mutations overall explain only about a quarter of inherited breast cancers.
“Just because you test negative for these three BRCA mutations doesn’t mean you’re in the clear, especially if you have a strong family history. You may need to decide if you want to undergo additional testing,” explains Kelly Morgan, a genetic counselor dedicated to this study. “This is just another illustration of why working with a trained healthcare provider is so important.”
Founders in the Field of Cancer Mutations
The three mutations included in the study — two in BRCA1 and one in BRCA2 — are called founder mutations. A founder mutation is a genetic change that appears with high frequency in a small group of people who were geographically or socially isolated for a long time and had ancestors who carried that specific gene mutation. Because Ashkenazi Jewish populations were culturally separated for hundreds of years, these BRCA mutations, which initially occurred by chance, became more common in that group.
In 1996, Dr. Offit and his team discovered the most common BRCA2 mutation linked to breast and ovarian cancers. The mutation has since been linked to other cancers, including prostate cancer and pancreatic cancer. Around the same time, other research groups identified the two BRCA1 founder mutations.
Teaming Up with the Community
Dr. Offit emphasizes that as a National Cancer Institute–funded cancer center, MSK counts treating the community in which it’s located as one of its primary roles. About two million people of Jewish descent live in the New York City metropolitan area, most of them Ashkenazi, and 20% of people treated at MSK have Jewish ancestry, making this focus especially fitting.
However, he notes, the information gained from focusing solely on this group in the BFOR study can later be applied to the wider population, just as other BRCA-related findings have been more broadly applied in the past.