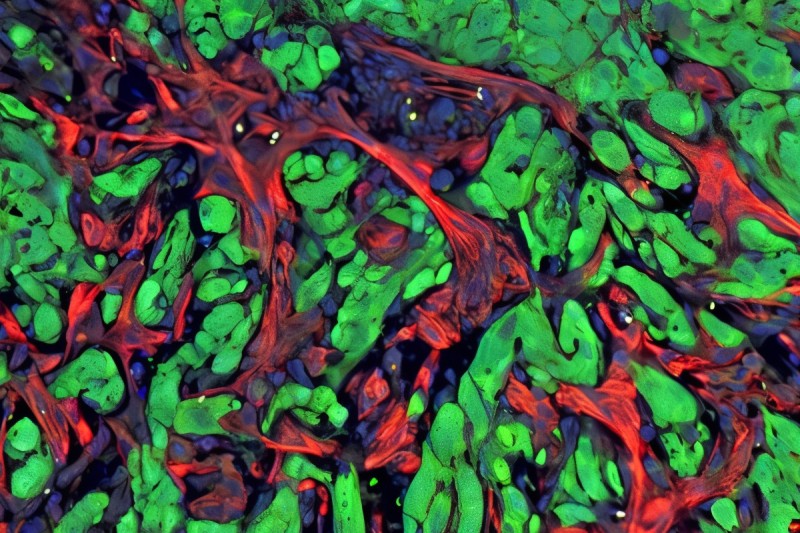
When it comes to cancer metastasis, it takes two to tango. That was one of the key findings of a new study led by researchers at Memorial Sloan Kettering Cancer Center (MSK): The TGF-beta and RAS signaling pathways work together to spur the spread of cancer in lung adenocarcinoma, a leading cause of cancer deaths around the world.
Take away one of those two signals, and lung cancer will not be able to spread (metastasize) to new parts of the body, their findings in animal models suggest.
The research, published September 6 in Cell, points to new opportunities to potentially prevent metastasis, thanks to an updated understanding of the underlying processes.
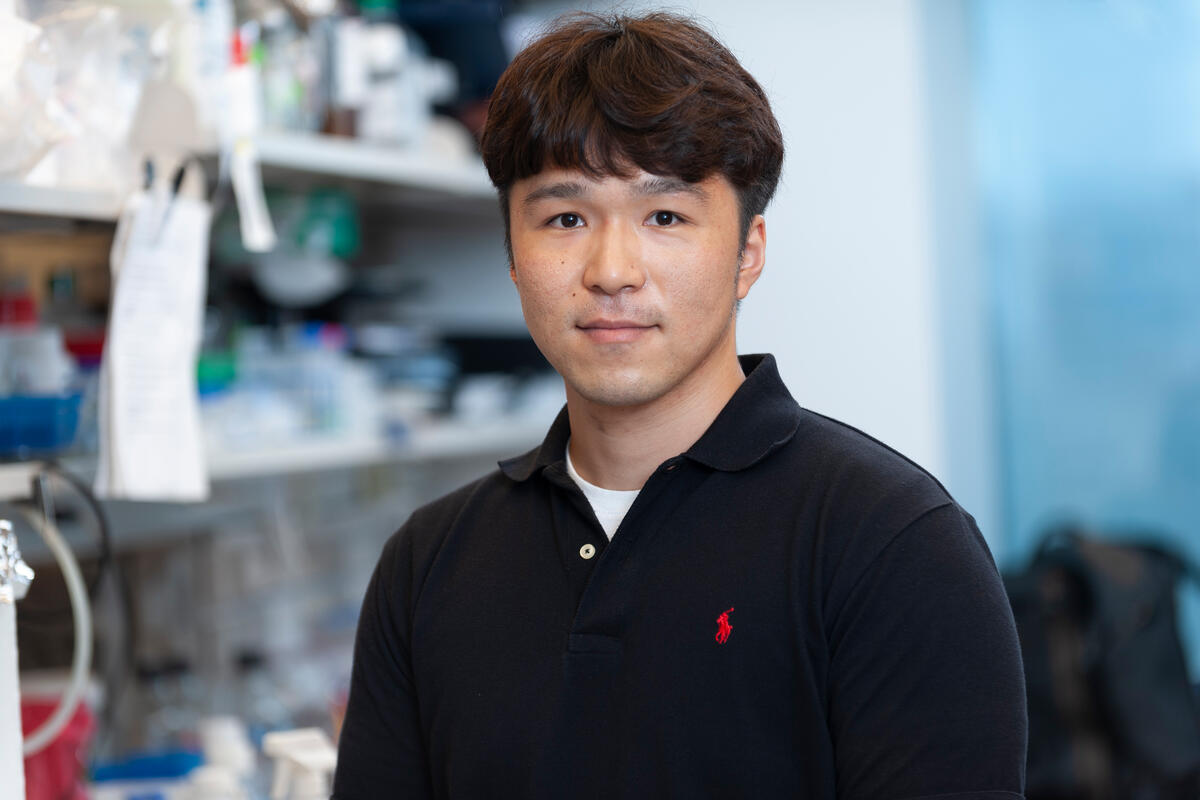
“About 9 in 10 deaths from cancer are caused by metastasis,” says Jun Ho Lee, PhD, the study’s first author and a postdoctoral researcher in the lab of senior study author Joan Massagué, PhD. “So research to understand, prevent, and treat metastasis has great potential to improve the lives of many people.”
A Tale of Two Signaling Pathways: TGF-Beta and RAS
On its own, TGF-beta — a type of signaling protein known as a cytokine — is not an ideal drug target. That’s because it plays a variety of important roles throughout the body, making it nearly impossible to block without risking major side effects.
TGF-beta normally plays critical roles in programs regulating embryonic development and injury repair. But these programs also get activated in cancer cells during metastasis, giving otherwise immobile cells the ability to travel and to invade tissues.
Metastasis in this case, however, also requires inputs from the RAS pathway, the researchers found.
RAS’s normal role is to transmit signals from outside of a cell to the cell nucleus, where it activates genes that control cell growth, division, and differentiation.
Here, the researchers determined that a transcription factor (a protein that specifically regulates the activity of certain genes) that is controlled by RAS plays a critical role in metastasis. It’s known as RAS response element binding protein 1 (RREB1). They found that RREB1 collaborates with a signaling complex called SMAD4, which is controlled by TGF-beta. And inhibiting RREB1 disabled the metastatic process in mouse models, suggesting it could be a potential new drug target — both in lung cancer and in related diseases like lung fibrosis.
Why Context Is Key for TGF-Beta’s Role in Cancer Metastasis
The study brings together two longstanding areas of research for the Massagué Lab: TGF-beta signaling and metastasis.
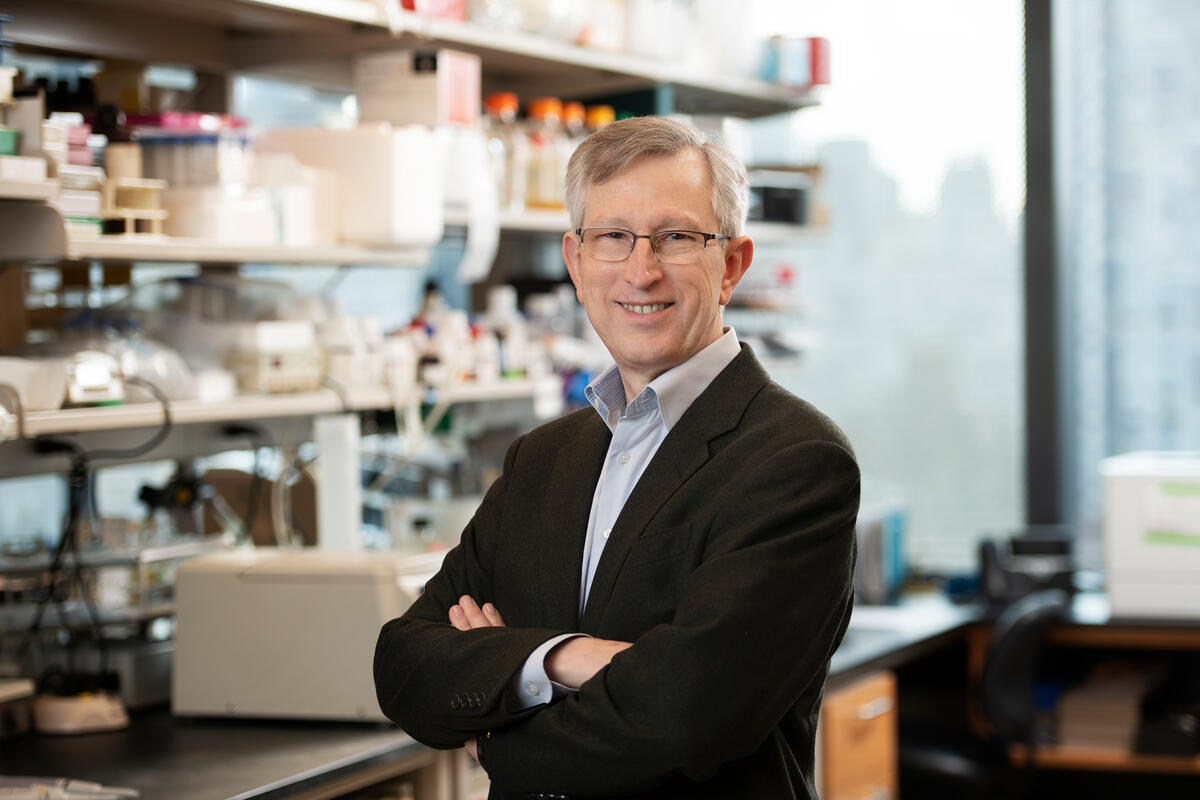
Dr. Massagué, who is Director of the Sloan Kettering Institute as well as MSK’s Chief Scientific Officer, is known for his pioneering work that uncovered the mechanism of action for transforming growth factor-beta (TGF-beta) signaling. The TGF-beta family of proteins plays a key role in the proliferation and differentiation of many different cell types, controlling the formation and regeneration of tissues from embryonic life to adulthood.
“We know that the TGF-beta pathway promotes injury repair and suppresses the formation of tumors in healthy tissues, but when tumors manage to grow, it promotes metastasis,” Dr. Massagué says. “So this is a big question we wanted to understand: How is it that metastasis can take something that is normally present to keep tissues healthy, turn it around, and use it to promote metastatic growth? And this has led to a whole program of research in my lab.”
Another way of putting it is that TGF-beta helps normal cells to regenerate, but when co-opted by cancer, this regeneration turns into runaway growth instead of healthy renewal.
In this study, the team shed new light on the mechanisms at work in the process, revealing that both RAS and TGF-beta inputs are needed for metastasis to take off — at least in this most common form of lung cancer, where the growth of fibrous scar tissue is a key component.
Beyond cancer, TGF-beta-driven lung fibrosis affects hundreds of thousands of people around the world. While targeting TGF-beta has been seen as promising, using TGF-beta inhibitors long-term to treat metastatic cancer or fibrosis might lead to significant side effects. For example, disrupting TGF-beta’s work can lead to excessive activity in the immune system, Dr. Massagué notes.
“So the biotech industry has been looking for ways to target TGF-beta only part-time or in restricted ways,” he says. “Here we’ve discovered a new candidate for that type of intervention, only focused on a partner signal that we now know is also required for metastasis and fibrosis.”
Further Understanding of Cancer’s Ability to Spread
The study is part of broader efforts across MSK to shed new light on how cancer progresses and spreads.
“In looking at the interactions between cancer and the environment where it grows — what we call the ‘tumor microenvironment’ — we are starting to uncover how cancer programs are driven by specific signals, involving pre-established response patterns that change the behavior of the cancer cell and of nearby cells,” Dr. Massagué explains.
In this instance, those nearby cells include collagen fiber-making fibroblasts.
Moreover, studies like this one that seek to understand the forces behind metastasis are further revealing how the overall maintenance and regeneration of tissues after an injury are tightly organized and orchestrated, Dr. Massagué says.
“We can then expand these understandings to other tumor types, to other organs in the body where metastases develop, to other forms of fibrosis,” he says.
Research That Can Only Happen at a Place Like MSK
The study also exemplifies the power of scientific collaboration and what’s possible at a place like MSK, where collaboration across scientific disciplines is a key facet of the culture, Dr. Massagué says.
For example, he says, Dr. Lee, the study’s first author, recruited scientific collaborators from across the Sloan Kettering Institute and Memorial Hospital to contribute toward aspects of the study that fell outside of the lab’s specializations.
“This project took several years, and before we knew where it was going to lead, the nature of the scientific questions Dr. Lee was asking about metastasis attracted other researchers,” Dr. Massagué says.
Additional Authors, Funding, and Disclosures
Additional authors include: Francisco Sánchez-Rivera, Lan He, Harihar Basnet, Fei Xavier Chen, Elena Spina, Liangji Li, Jason E. Chan, Digvijay Kumar Yarlagadda, Jin Suk Park, Carleigh Sussman, Charles Rudin, Scott Lowe, Tuomas Tammela, and Richard Koche of MSK; Carles Torner of the Barcelona Institute of Science and Technology; and Maria Macias of the Barcelona Institute of Science and Technology and the Institució Catalana de Recerca i Estudis Avançats.
This work was supported by National Institutes of Health grants (R35-CA252978, P01-CA129243, R01-CA270116, P30-CA008748); grants from the Alan and Sandra Gerry Metastasis and Tumor Ecosystems Center (GMTEC), the Agencia Estatal de Investigación, Ministerio de Ciencia e Innovación (PID2021-122909NB-I00), European Regional Development Fund (ERDF), and Agilent Technologies; and fellowships from the Josie Robertson Foundation, the American Cancer Society, the Rita Allen Foundation, the V Foundation, GMTEC, the Translational Research Oncology Training Program, the Damon Runyon Cancer Research Foundation, and the Agency for Administration of University and Research Grants (AGAUR). Additional support was provided by the Fiona and Stanley Druckenmiller Center for Lung Cancer Research and the Robert J. Kleberg, Jr. and Helen C. Kleberg Foundation. The researchers also acknowledge the Ministerio de Ciencia e Innovación through the Centers of Excellence Severo Ochoa Award, the BBVA Foundation, and the CERCA program of the Government of Catalonia.
The researchers report various pharmaceutical industry investments and consulting work unrelated to this study. A full listing can be found in the journal article.
Read the article: “TGF-β and RAS jointly unmask primed enhancers to drive metastasis,” Cell. DOI: 10.1016/j.cell.2024.08.014