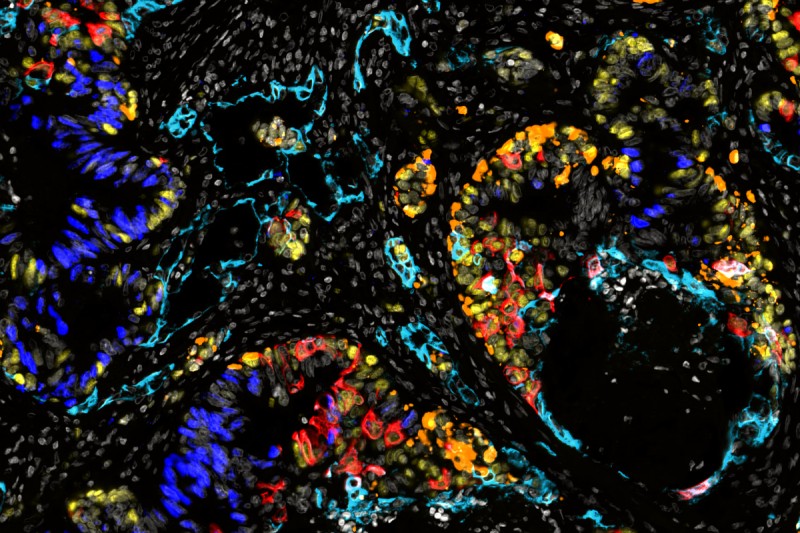
Fluorescent image of of a patient’s colorectal cancer liver metastasis showing the diversity of cell states from normal intestinal states (dark blue) to atypical cell states (other colors). Image credit: Elizabeth Benitez
Metastasis remains the primary challenge to reducing cancer deaths worldwide, says Memorial Sloan Kettering Cancer Center (MSK) gastrointestinal oncologist Karuna Ganesh, MD, PhD. That’s when a primary tumor — colorectal cancer, for example — spreads to a new part of the body, such as the brain, liver, or bones.
The new tumor is still colorectal cancer (not brain, liver, or bone cancer), yet the cells in the new tumor are also radically different from those in the tumor where the cancer started. And the differences between the two are critical.
Dr. Karuna Ganesh
“Sometimes we say that people don’t die from cancer, they die from metastasis,” Dr. Ganesh says. “We know how to cure primary tumors — with surgery, and sometimes with chemotherapy and radiation. Metastatic disease, too, will often respond to first-line therapy, but you can never get rid of all the cancer cells completely. The cancer cells that survive treatment become more and more aggressive, and eventually you can’t stop them.”
Effective treatments against metastasis will require a deeper understanding of both the changes that happen when cells from a primary tumor metastasize and the mechanisms that drive those changes, she adds.
Now a new MSK study, published October 30 in Nature, overseen by Dr. Ganesh and MSK computational biologist Dana Pe’er, PhD, is providing unique insights into metastasis that researchers say point to new therapeutic opportunities.
Study Illuminates Differences Between Primary and Metastatic Colorectal Cancer
The scientists’ findings provide new details about metastatic cancer cells’ ability to “time travel” back to earlier, flexible states seen in embryonic development — what scientists call “cellular plasticity.”
Plasticity refers to the ability of cancer cells to shed their identity as, say, intestinal cells and to return to a primordial state that can give rise to completely different cell types: skin-like cells (squamous), bone-like cells (osteoblasts), and cells that release hormones and communicate with the nervous system (neuroendocrine).
By comparing samples from patients with advanced colorectal cancer, the research team identified clear patterns in the way metastatic cells reprogram themselves to access these early cell states.

Dr. Dana Pe’er
“Rather than focusing on genetic mutations that give rise to cancer in a primary tumor, what we focused on here is cancer cells’ ability to change their identity during metastasis — for a cell that started out as an intestinal cell to become a completely different type of cell by accessing programs that are typically only available during the earliest stages of human development,” says Dr. Pe’er, who is also a Howard Hughes Medical Institute Investigator.
The effort required innovative thinking, sophisticated experimental and computational expertise, and extensive collaboration between oncologists, surgeons, and laboratory researchers with a variety of specializations — enabled by the breadth and depth of expertise at MSK, the collaborative culture, and the volume and nature of the cases that MSK researches see, the researchers say.
The study was led by co-first authors Andrew Moorman, MS, a computational biologist in the Pe’er Lab, and Tri-Institutional MD/PhD student Elizabeth Benitez and postdoctoral fellow Francesco Cambuli, PhD, both from the Ganesh Lab.
Studying Metastasis Using Three Kinds of Tissue
The researchers collected a trio of samples from each of 31 patients — from their primary tumor, nearby healthy tissue, and metastatic tissue (usually from the liver).
The researchers then used single-cell RNA sequencing, advanced immunofluorescence microscopy, and organoids (miniature lab-grown model organs) generated from the samples to study the cancer cells’ evolution during metastasis.
The study included patients who had not yet received any cancer treatment, as well as those who had received chemotherapy before surgery. Some patients had additional samples collected at a later time.
Analyzing matched trios of tissue from a group of patients is an innovative way to get insights into one of cancer’s biggest challenges. Standard laboratory models, such as cell lines or mice, can’t readily answer key questions about why metastasis gains such aggressive capabilities that eventually kill, which primary tumors alone usually don’t, the researchers say.
Mouse models of cancer often don’t metastasize, and when they do, the process is greatly accelerated compared with how cancer evolves in people — which means they’re not particularly accurate for understanding the development of plasticity in human cancers on human timescales, Dr. Pe’er says.
“We thought it was really important to look at the disease for which we need better treatments, which is advanced cancer in humans,” Dr. Ganesh says. “So we had to get a little creative, because when patients get metastatic disease, we don’t often perform surgeries to cut it out.”
Moreover, surgery is a very specialized field. Surgeons do sometimes take out part of the liver to remove a metastasis, but generally a different surgeon would operate on the colon to remove a primary tumor.
“So we really had to bring together a broad, collaborative group to collect and study these different samples during one surgery,” Dr. Ganesh adds. “What we’ve been able to achieve — to be able to look at normal tissue, primary tumor, and metastasis from the same patients at the same timepoint — has never been done at this scale before.”
Toward a Deeper Understanding of Metastasis
The transition of healthy cells to primary tumors in colorectal cancer has been well studied. During this transformation, tumor cells adopt the properties of intestinal stem cells, which renew and repair intestinal tissue. This is their first journey back in time to a more primitive state.
The new study shows for the first time — and contrary to the accepted wisdom — that metastatic colorectal cancer cells don’t look like the intestinal stem cells found in the primary tumor. Instead, the more metastatic cells divide and evolve over time, the more they lose their original identity as intestinal cells.
A sophisticated computational analysis revealed a clear pattern:
“Despite all the normal variation we see from one patient’s cancer to the next, the cells in every patient’s tumors converge on a fetal-like state,” Dr. Pe’er says.
This state very closely resembles the primordial endoderm — the cells that eventually give rise to the intestines in the first trimester of embryonic development.
From there, metastatic cells travel even further back in time — back to a point before they’re locked into becoming intestinal cells and can instead become skin or bone or nerve cells.
“The signature we found very closely resembles what happens in week 6 during development,” Dr. Pe’er says. “Week 6, day 6.6, to be precise.”
Implications for Treating Metastatic Cancer
All this time traveling that cancer cells do is a survival mechanism, an adaptation to help them survive stress — especially the assaults of cancer treatments, Dr. Ganesh says.
Across patients, the metastatic cells all travel back to the same point in time, where they can activate gene programs associated with a variety of cell types, which allows them to gain the ability to metastasize to diverse tissues and makes them more resistant to cancer drugs.
“From a clinical standpoint, we think this is profoundly important,” Dr. Ganesh says. “If there’s a specific state that these cells need to enter, in order to regenerate a tumor after therapy, this is a bottleneck — a vulnerability.”
This discovery presents opportunities to target cancer cells’ ability to enter this primordial state, as well as to target the state itself, Dr. Ganesh says. Research into both approaches is ongoing at MSK.
What Organoids Are Teaching MSK Researchers
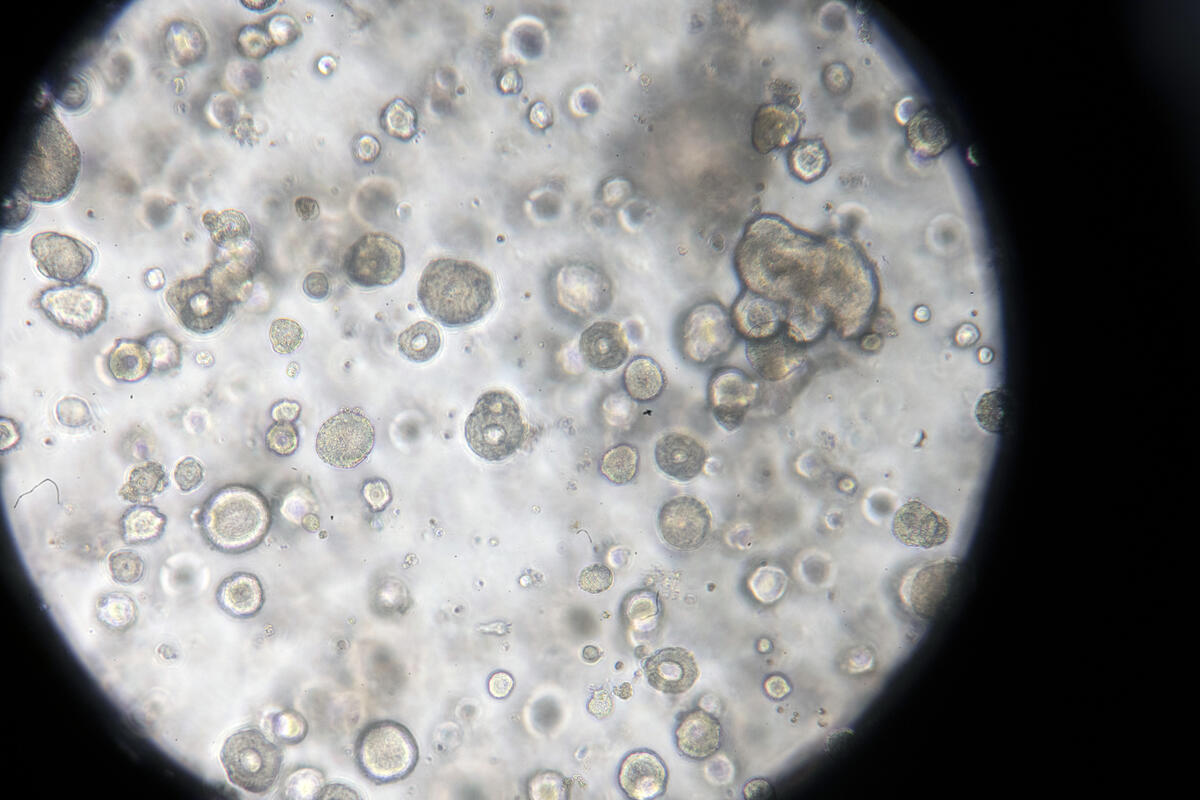
Patient-derived colorectal cancer organoids under the microscope.
This is also where the organoids created from the matched patient samples are providing insights that wouldn’t be possible using other methods.
“We now know that metastatic and primary cancer cells are different, but the organoids really allow us to ask, ‘Why are they different?’ ” Dr. Ganesh says. “Are they responding to different cues in the liver versus in the colon?”
It turns out that primary tumor cells that originate in the colon can only live in the colon; they can’t adapt to the environment in the liver. Metastasis cells, on the other hand, can survive in both the colon and in the liver.
“So that tells us that they have greater plasticity,” Dr. Ganesh adds. “This research is really the first demonstration that there is a type of plasticity at work in metastatic cells that allows for this adaptation to different micro-environmental cues.”
Ultimately, the team is optimistic that their findings can provide a roadmap to further understanding metastasis and eventually to targeting cellular plasticity in advanced cancers.
Additional Authors, Funding, and Disclosures
The study was a collaboration involving 39 authors from across MSK and the Tri-Institutional graduate programs that span Weill Cornell Medicine, Rockefeller University, and MSK. Please refer to the journal article for the full list.
The work was supported by grants from the National Institutes of Health (U2CCA233284, U54CA209975, R37CA266185, K08CA230213, T32GM007739, U01CA23844401A1, R01EB027498A1, P30CA008748), a Gilliam Fellowship, the National Science Foundation Graduate Research Fellowship Program, a Damon Runyon Clinical Investigator Award, a Burroughs Wellcome Career Award for Medical Scientists, an American Association for Cancer Research NextGen Grant for Transformative Cancer Research, a Stand Up to Cancer Convergence 3.1416 Award, the Pershing Square Sohn Prize, the Starr Cancer Consortium, a Josie Robertson Investigator Award, a Barbara and Stephen Friedman Predoctoral Fellowship, and Alan and Sandra Gerry Metastasis and Tumor Ecosystems Center grants.
Dr. Ganesh is an inventor in U.S. Patent 11,464,874, and U.S. Provisional Patent Applications 63/478,809 and 63/478,829 on targeting L1CAM to treat cancer, submitted by Memorial Sloan Kettering Cancer Center. Dr. Pe’er is on the scientific advisory board of Insitro. Co-author Jinru Shia, MD, is a consultant for Paige AI. Rona Yaeger, MD, has served on the advisory board for Pfizer, Mirati Therapeutics, Revolution Medicine, Loxo@Lilly, and Amgen, received a speaker’s honorarium from Zai Lab, and has received research support from Pfizer, Boehringer Ingelheim, Mirati Therapeutics, Daiichi Sankyo, FogPharma, and Boundless Bio. Julio Garcia-Aguilar, MD, PhD, owns stock in Intuitive Surgical. Ronan Chaligné is a consultant for Sanavia Oncology, S2 Genomics, and LevitasBio. All other authors declare no competing interests.
Read the study: “Progressive plasticity during colorectal cancer metastasis,” Nature. DOI: 10.1038/s41586-024-08150-0