Genitourinary oncologist Jonathan Rosenberg says two newer classes of bladder cancer drugs are greatly expanding treatment options for the disease.
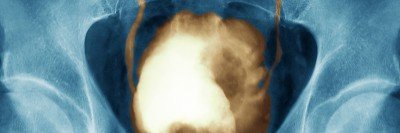
Promising new drugs have begun to transform the treatment of bladder (or urothelial) cancer, the sixth most common form of the disease in the U.S., and the fourth most common in men. In particular, two drug classes, antibody-drug conjugates (ADCs) and checkpoint inhibitors, are giving patients much-improved treatment options for various stages of bladder cancer.
Now a new treatment approach combining these therapies has shown positive results in a clinical trial for people with metastatic bladder cancer. The trial tested the effectiveness of the antibody-drug conjugate enfortumab vedotin (Padcev®) combined with the checkpoint inhibitor pembrolizumab (Keytruda®).
This treatment had already received Breakthrough Therapy Designation from the U.S. Food and Drug Administration (FDA) in 2020. The promising new clinical trial results are expected to lead to an accelerated approval for this drug regimen as a first-line treatment for people with metastatic bladder cancer who cannot receive cisplatin-based chemotherapy, the standard first-line treatment.
“Although bladder cancer cases are going down, the death rates haven’t changed significantly,” says Memorial Sloan Kettering Cancer Center (MSK) genitourinary oncologist Jonathan Rosenberg, who presented the trial results on September 12, 2022, at the annual meeting of the European Society for Medical Oncology (ESMO). “Having these new treatment options available brightens the outlook considerably for many bladder cancer patients. While immunotherapy has gotten more attention in recent years, antibody-drug conjugates might end up making the bigger positive impact, at least in the near future.”
Antibody-Drug Conjugates Deliver a Precise Payload
Antibody-drug conjugates work to treat cancer by combining three parts:
- An antibody that binds to specific proteins or receptors on the surface of the cancer cell
- A drug, such as chemotherapy, that is toxic to the cancer cell
- A linker that connects the drug and antibody, keeping the drug bound to the antibody and shielded from the body until it arrives at the cancer cell
This formulation selectively delivers the drug to the cancer cells, destroying them while sparing normal body parts from high doses of the drug.
Clinical Trial Testing Enfortumab Vedotin Shrinks Bladder Tumors
Enfortumab vedotin binds to a protein on bladder cancer cells called nectin-4 and delivers a chemotherapy drug called monomethyl auristatin E. Dr. Rosenberg previously led multiple clinical trials resulting in FDA approval of enfortumab vedotin in 2019 for people with locally advanced or metastatic bladder cancer who cannot have surgery or whose disease persists despite prior treatment with immunotherapy and chemotherapy.
At the ESMO meeting, Dr. Rosenberg reported results from a phase 2 trial of enfortumab vedotin given in combination with pembrolizumab to people newly diagnosed with metastatic urothelial cancer who are unable to receive cisplatin chemotherapy. This combination therapy shrank tumors in 64.5% of patients, which appears much better than standard chemotherapy treatments such as gemcitabine and carboplatin. In addition, 10.5% of patients had their tumors disappear completely on imaging tests.
“These are remarkable results that could make a big impact in treating metastatic bladder cancer,” Dr. Rosenberg says. “The results of this trial confirm the findings of a smaller study testing the same combination.”
The drug combination is being investigated for other patient groups as well. MSK is taking part in a phase 3 clinical trial, led at MSK by medical oncologists Gopa Iyer and Samuel A. Funt, testing enfortumab vedotin combined with pembrolizumab as the initial treatment, compared with standard chemotherapy in people with inoperable or metastatic urothelial cancer.
In another trial, Dr. Rosenberg and genitourinary oncologist David Aggen are testing enfortumab vedotin and pembrolizumab in patients whose cancers have spread beyond the bladder to the pelvic lymph nodes. In this trial, patients get about 4.5 months of treatment prior to planned surgery to remove the bladder and pelvic lymph nodes, with the hope of significantly increasing cure rates in this difficult-to-treat patient population.
Another ADC, sacituzumab govitecan, has been approved for locally advanced or metastatic bladder cancer, based on clinical trials led by other institutions.
“We expect more ADCs to come out of the pipeline, and we’ll continue exploring ways to combine them with other drugs, such as checkpoint inhibitors, to make them even more effective,” Dr. Rosenberg says.
Checkpoint Inhibitors Unleash an Immune Attack
Checkpoint inhibitors work by releasing a natural brake that the immune system places on powerful immune T cells so they don’t accidentally attack normal cells. Since 2016, four checkpoint inhibitor drugs have been approved for bladder cancer: atezolizumab (Tecentriq®), pembrolizumab (Keytruda®), nivolumab (Opdivo®), and avelumab (Bavencio®).
The drugs target molecules called PD-1 or PD-L1, which are on the surface of immune T cells or on cancer cells. MSK played a key role in gaining FDA approval for atezolizumab, pembrolizumab, and nivolumab.
MSK genitourinary oncologist Dean Bajorin led a large international clinical trial showing that nivolumab reduces bladder cancer recurrence in people whose disease has spread into the muscle wall. About 25% of bladder cancers fall into this high-risk category, which is harder to treat and much more likely to spread to other parts of the body. The FDA approved nivolumab for this use in 2021.
“The absence of good options to treat high-risk disease was frustrating for both patients and doctors,” Dr. Bajorin says. “Now, for the first time, we can offer a new immunotherapy to reduce recurrence. It’s a major advance.”
Here’s how the other FDA-approved drugs help patients:
- Pembrolizumab can be given for locally advanced or metastatic bladder cancer that resists standard chemotherapy drugs.
- Pembrolizumab or atezolizumab can be given to people too sick to receive chemotherapy.
- Atezolizumab can be given to people who have metastatic bladder cancer with high levels of PD-L1 that has not been previously treated and who also cannot receive cisplatin chemotherapy.
Researchers are also gaining a better understanding of who is likely to respond to these drugs and how to make them work better in combinations.
“The emergence of checkpoint inhibitors has been a revolution for some people who have highly aggressive, life-threatening bladder cancer,” Dr. Rosenberg says. “But immunotherapy still doesn’t work in enough patients. We have to find better ways to improve response rates and survival. Even if checkpoint inhibitors and antibody-drug conjugates don’t represent a cure for bladder cancer, anything that could help people live longer or delay progression of the disease — in some cases, allowing them to avoid bladder removal or chemotherapy after surgery — will improve their quality of life.”
Key Takeaways
- New drug types are being used to treat bladder cancer, especially metastatic bladder cancer.
- Antibody-drug conjugates carry anti-cancer drugs directly to tumor cells.
- Checkpoint inhibitors enable the immune system to attack cancer.
- These drugs, especially when combined, show promise for treating bladder cancer at various stages.