Long before Louis Pasteur became famous for proving that diseases were caused by germs, he worked in a beer factory. His job: finding a way to make beer from sugar, hops, and yeast without having the yeast take over the vat, gunking up the beer.
He failed.
Turns out yeast are very good at converting sugar into more yeast, and nothing Pasteur did could change that — which is why today, most beer is filtered.
This long-familiar fact about beer making is inspiring some unconventional thinking about cancer. In a paper published today in Cell Metabolism, Memorial Sloan Kettering President and CEO Craig Thompson and postdoctoral fellow Natasha Pavlova argue that cancer cells take up and use nutrients much like yeast in a vat of sugar, reproducing with wild abandon. Further, they claim that it’s this altered metabolism of nutrients — rather than any quirk of a disordered cell cycle — that lies at the heart of cancer.
“All of the information that drives the cell cycle — drives cell growth — comes from cells recognizing that they have adequate nutrients,” says Dr. Thompson.
If he’s right, then much of what we think we know about cancer is wrong.
The Challenges of Living Together
For Dr. Thompson and his colleagues, the problem of cancer is intimately tied up with another biological question: how living things evolved from single-celled organisms, such as yeast, to multicellular organisms like fish, birds, and biologists.
“The fundamental thing that allows us to live as a collaborative multicellular organism — a society of cells — is that every cell agrees it will not take up and utilize the shared resources available to the body except on its instruction from other cells,” says Dr. Thompson.
In this view, cancer results when cells stop playing by the food rules. Through mutations, they develop the capacity to acquire nutrients autonomously. After that, it’s every cell for itself.
The easiest way to see this, Dr. Thompson says, is to consider what happens when a person gets a yeast infection in the blood, a common problem on hospital wards where people are often immunocompromised. The yeast find their way from the bloodstream to the liver — a nutrient smorgasbord — and grow out of control.
“Metastatic cancers do the same thing,” he explains. “They act just like yeast, and that’s why the liver is the most common site of metastasis.”
Revisiting Cancer’s Hallmarks
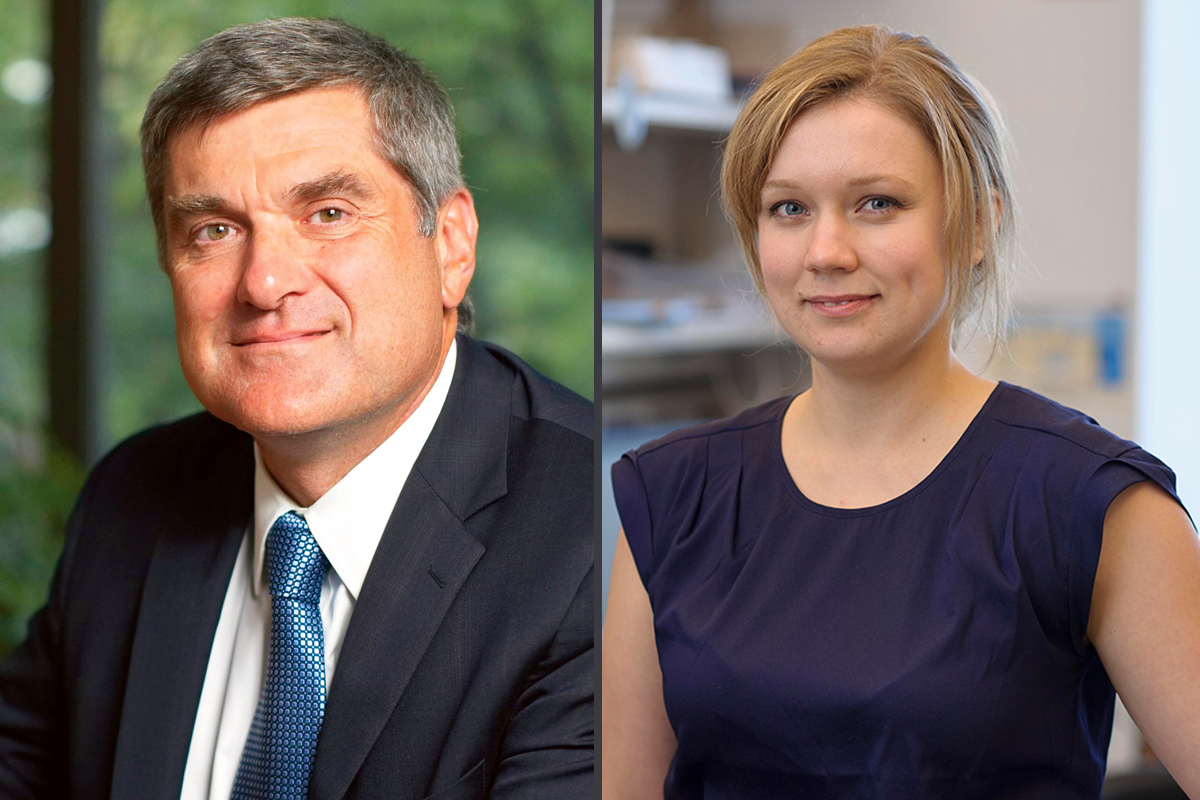
Drs. Thompson and Pavlova named their paper “The Emerging Hallmarks of Cancer Metabolism” in homage to a famous article called “The Hallmarks of Cancer,” published in 2000 by Douglas Hanahan of UCSF and Robert Weinberg of MIT.
In that article — required reading for every cancer biologist — the authors describe six features, or hallmarks, of cancer that they believe characterize the disease, including things like activated growth factor signaling and evasion of cell death. Not included on the list is anything having to do with altered metabolism, the subject of the new paper.
Metabolism did later receive attention from these authors, but even then it was accorded a secondary status.
“The repeated refrain from traditional biochemists is that altered metabolism is merely an indirect phenomenon in cancer, a secondary effect of cancer cells gaining signals to survive and proliferate,” Dr. Thompson says. “The heretical part of our argument is that we’ve gotten all of this wrong.”
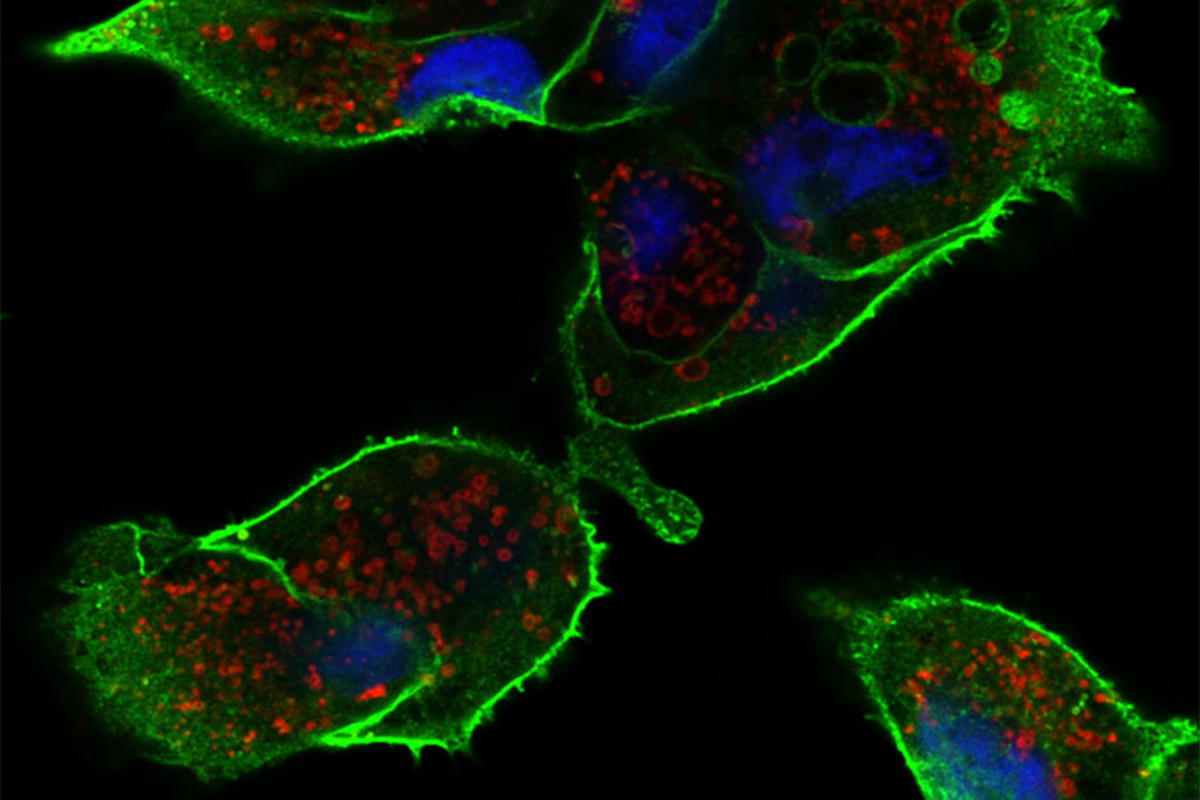
In support of their view, Drs. Thompson and Pavlova point out that many cancer-causing genes, or oncogenes, have direct effects on metabolism. For example, the oncogenes AKT and RAS directly increase glucose consumption by cells. Other cancer-associated genes, such as MYC and Rb, boost uptake of amino acids, another important nutrient.
“It is becoming increasingly clear that oncogenes do not simply transmit instructions for a cell to survive, grow, and divide, but in fact directly control nutrient uptake and utilization,” says Dr. Pavlova, a postdoctoral fellow in the Thompson lab and the paper’s first author.
This “metabolic reprogramming” has long-term consequences for the cell, she says, transforming it from one that obeys the instructions of its neighbors to one that seeks only to feed and reproduce itself.
Rediscovering Metabolism
The new theory helps to make sense of a long-standing cancer conundrum. Scientists have known since the 1920s that cancer cells take up much more glucose than normal cells (which, incidentally, is the basis for PET scans). However, cancer cells don’t process this sugar in the same way normal cells do.
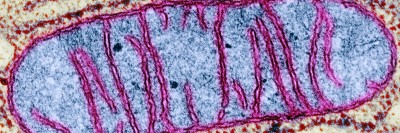
Typically, cells burn sugar in their mitochondria to make ATP, which they use to power chemical reactions. (Recall from your high school biology class that mitochondria are the cell’s “power plants.”) Cancer cells, on the other hand, use the less efficient process of glycolysis, which produces fewer molecules of ATP and leaves much of the glucose energy untapped. This type of metabolism has been dubbed “the Warburg effect,” after Otto Warburg, who first observed it. But it’s not specific to cancer. Yeast do this too; it’s called fermentation.
This fact has perplexed biologists over the years, since cancer cells presumably have a great need for energy. “For a hundred years, we’ve thought that the whole problem of life was gaining a battery supply,” Dr. Thompson says. “We weren’t thinking about the problem of how you actually make two of something.”
To make two (and four and eight) of themselves, cancer cells need more than just energy; they need building materials — sugar to construct DNA and lipids to make membranes, for example. Shunting nutrients from the power plant to the assembly line, therefore, makes perfect sense.
The effects of cancer metabolism do not end there. Metabolic products also affect gene expression, which shapes a cell’s identity. Cancer cells even pump out metabolic products that trick neighboring normal cells into helping them proliferate and spread.
New Treatment Options
If correct, Drs. Thompson and Pavlova’s new theory suggests that targeting altered metabolism could be an effective approach to cancer treatment. Drugs not previously thought of in the context of cancer — such as the diabetes drug metformin — might become useful in the fight against the disease. We might even find that many existing cancer drugs, including certain targeted therapies, achieve their effects by affecting a cell’s access to nutrients, in contrast to current theories of how they work.
The study of cancer metabolism is more than a century old, but these recent discoveries are revitalizing interest in the subject. Asked if he thinks the time will come when altered metabolism will be seen as a full-fledged cancer hallmark, Dr. Thompson is bullish: “I actually don’t think it’s a hallmark of cancer,” he says. “I think it’s the root cause.”