Molecular geneticist Elli Papaemmanouil and other scientists found that acute myeloid leukemia is not one disorder but at least 11 distinct subtypes caused by specific genetic changes.
Acute myeloid leukemia (AML), an aggressive blood cancer, has proved to be tricky for doctors to assess and treat. Patients vary widely in their response to treatment, and clinicians have found it nearly impossible to predict who will do well and who will fare poorly.
A new study analyzing more than 100 genes known to cause the disease reveals a major reason for this disparity: AML is not one disorder but at least 11 distinct subtypes caused by specific genetic changes. This discovery could change the way patients are diagnosed and treated.
“These findings help us understand how AML develops as mutations occur — what the critical events are that fine-tune the leukemia,” says Memorial Sloan Kettering molecular geneticist Elli Papaemmanuil, who co-led the study, which was published today in the New England Journal of Medicine (NEJM). “This is the first step in helping us to identify who needs aggressive treatments and to choose who might benefit from clinical trials.”
The study was conducted in collaboration with the Wellcome Trust Sanger Institute and a team of international colleagues. It involved analyzing leukemia-associated genes in 1,540 AML patients enrolled in three clinical trials in Europe — the largest AML patient group ever used for this type of genetic study. Researchers looked for common genetic themes behind development of the disease. They found that patients fit into at least 11 major groups, each with different assortments of genetic changes and distinctive clinical features.
“For the first time, we untangled the genetic complexity of AML genomes into distinct genetic subgroups, reflecting paths leading to specific subtypes of AML,” Dr. Papaemmanuil explains. “This enables us to understand the biology of AML types and to use that information to develop clinical approaches such as combination therapies for clinical trials based on the mutation patterns.”
Mutational Profiles and AML Subtypes
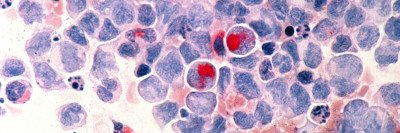
AML is characterized by the rapid growth of abnormal white blood cells. It develops when precursor cells in the bone marrow become cancerous as a result of a series of errors in the DNA. This usually requires mistakes in several key genes controlling blood-cell production. The disease affects people of all ages and often requires months of intensive inpatient chemotherapy.
Although in recent years researchers have identified a handful of AML mutations that play a significant role in driving the disease, most patients have a number of additional mutations that may or may not be important. The new study clarifies how the interplay between many of these mutations can affect the disease’s progression.
MSK leukemia researcher Ross Levine, in an accompanying NEJM editorial, cited Robert Frost’s “The Road Not Taken” in describing how distinct paths — initiated by varying mutations — lead to different disease destinations. The study, he wrote, provides “an unprecedented understanding of the different roads that lead to AML and how the specific path from normal blood cell to leukemia has important biologic and clinical implications.”
In the study, full knowledge of the genetic makeup of a patient’s leukemia greatly improved clinicians’ ability to predict whether that patient would be cured with current treatments.
Because the study was so large, it allowed researchers to tease out genetic interactions that were not previously recognized. For example, the analysis showed patterns not just in the combination of mutations that occur but also in how one mutation can lead to a subsequent aberration.
“Once you expand to a large cohort, you identify relationships, not just in the combination of which mutations come together but also in the order in which they’re acquired,” Dr. Papaemmanuil says.
“This work provides us with a blueprint for how leukemia develops,” Dr. Levine adds. “It shows that how that blueprint is written really matters for the patient.”
Validating Genomic Analysis
The study illustrates the promise of improving cancer care through genomic analysis of patient-derived samples.
The Marie-Josée and Henry R. Kravis Center for Molecular Oncology, established at MSK in 2014, is taking this approach by correlating molecular information from tumors with clinical data, including patients’ outcomes and responses to therapy.
More specifically, MSK’s newly established Center for Hematologic Malignancies seeks to use this type of molecular data to better understand how leukemia develops — and then to apply those findings to crafting better therapies.
“This gives us a framework to go back to the lab and understand how all this wiring contributes to leukemia — to really look under the hood,” Dr. Levine says. “This is the basis for scientific studies to unlock new ideas about this disease and to test new therapeutic ideas.”