This information describes what a continuous glucose monitor (CGM) is and how to use and place it. It also explains how to read glucose levels and care for your CGM.
What is a continuous glucose monitor?
A CGM is a small, wearable device that measures your glucose (sugar) level every few minutes. It is made up of a sensor and a transmitter.
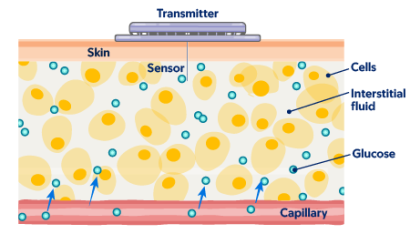
The sensor is a small filament (fiber) that goes into your skin and measures your glucose (see Figure 1). The transmitter sits on your skin and sends data to a device reader or an app on your smartphone. This lets you track your glucose level using fewer fingersticks (fingerpricks).
- Check your glucose levels at any time.
- See how physical activity and food affect your glucose in real time to make healthy lifestyle choices.
- Easily share reports with your care team, including your healthcare provider and caregivers.
Who can use a CGM
Anyone can use a CGM, but you’ll need a prescription to get one. CGMs are most often used by people with type 1 diabetes or type 2 diabetes who use insulin.
Insurance coverage for CGMs
Usually, insurance will only pay for the device if you take more than1 insulin injection a day. If insurance does not cover it, you can pay for it on your own. Talk with your healthcare provider to learn more.
Ask about your medications
Certain medicines, such as acetaminophen (Tylenol®) or hydroxyurea (Droxia®), can cause less accurate CGM readings. Talk with your healthcare provider about which medicines are safe to take while using a CGM.
How to use a continuous glucose monitor
There are several kinds of CGM systems. Most work in the same way. Talk with your healthcare provider about which one is right for you.
Your outpatient diabetes care team will help teach you how to use the CGM system they prescribe for you. Read the product user guide, including safety information and how to use your CGM. You can also go to the manufacturer’s website or contact customer support for help with your device.
How and where to place your CGM
Use the applicator to place the CGM onto the back of your upper arm or your belly. Follow the instructions that come with your specific CGM system. Avoid placing the CGM over scars, moles, stretch marks, or areas where you inject insulin.
The CGM has a sticky backing to keep the sensor in place on your skin. You can also use a CGM cover to help protect and keep it in place. Avoid using lotion or powder near the sensor. They can keep the sensor from sticking to your skin.
You can place a CGM cover over your device to help keep it from falling off. Do not cover the sensor with the sticky part of the covering. This can trap water in the sensor and damage it. You can buy these coverings at your local pharmacy or online.
How to read your glucose measurements
CGM readings may be different from fingerstick readings. Fingersticks measure your glucose level from your bloodstream. A CGM measures your glucose from interstitial (IN-ter-STIH-shul) fluid. This is the fluid between your body’s cells (see Figure 2).

CGM versus fingerstick glucose readings
Glucose levels in your interstitial fluid change slower than in your bloodstream. Blood glucose (BG) reading from a fingerstick will show your blood glucose level in real time. Your CGM sensor glucose (SG) reading may show what your glucose was up to 15 minutes ago. It’s normal for these readings to be slightly different, even if your glucose is stable (not changing).
If your glucose is changing quickly, it’s normal to see a bigger difference between blood and CGM sensor glucose readings. This can happen right after you’ve eaten. Your sensor will tell you if your glucose is out of range. Call your diabetes healthcare provider if you have any concerns.
Read the “How to read your glucose level using a continuous glucose monitor” section below to learn more.
How to read your glucose level using a continuous glucose monitor
Your glucose level changes throughout the day. The CGM will measure your glucose level every few minutes. It will send the data to the device reader or your smartphone app wirelessly by Bluetooth. Make sure your reader or smartphone is close by at all times.
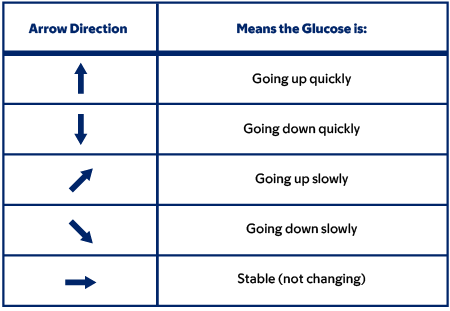
A program in the reader or app uses the data to show you a trend with an arrow or arrows (see Figure 3). This lets you know if your glucose is changing or in a stable pattern. If your glucose is changing, it will tell you how quickly it is going up or down.
Things that affect your glucose readings
Many things, including physical activity and food, can cause your glucose levels to change. You can use your CGM glucose readings to make healthy lifestyle choices and prevent problems caused by diabetes. For example, certain activities or foods can help keep your glucose in the target range longer. The target range is when your glucose is not too high or too low.
Talk with your healthcare provider about what your target range is and which activities and foods are best for you.
When to do a fingerstick to measure glucose
Fingersticks are an important part of managing your diabetes. Doing a fingerstick can help confirm if your CGM glucose reading is correct. This helps you decide how to manage your glucose. Always have your blood glucose meter and testing supplies available.
You do not have to regularly check your blood glucose by fingerstick while using a CGM. Do a fingerstick if you feel like your CGM glucose reading does not match how you feel. For example, you may feel symptoms of hypoglycemia even though your glucose reading is in the target range.
- Too high
- Too low
- Changing very quickly
How to care for your continuous glucose monitor
Bathing and showering
It is safe to shower or take a bath with your CGM in place. Many CGMs are water resistant, but not waterproof. Follow the instructions that come with your CGM before swimming.
Using your continuous glucose monitor while you’re staying at MSK
If you need to stay at MSK, you can keep your CGM on for your information and comfort. If you choose to keep it on, your healthcare provider will ask you to sign a form. This form describes the terms of agreement that let you to keep the CGM on while you’re in the hospital. For your safety, we ask that you agree to these terms or take off the device.
Your care team will use a fingerstick to check your blood glucose level in your hospital room. Your results will appear right away on the hospital’s blood glucose meter. This is called point-of-care testing (POCT). Your care team will use POCT to make any decisions about treatment, such as medication doses, tests, or procedures.
If you choose to use your CGM while you’re in the hospital, you must care for it during your stay. If you have a CGM reading that is outside the normal range, call the nurse right away. They will use POCT to confirm the reading and guide your treatment.
You’ll need to bring your own supplies, including replacement CGMs and coverings. MSK cannot:
- Fill your CGM prescription.
- Reimburse you for a replacement CGM if you lose it or you have to take it off as part of your care.
To learn more, read Using Your Insulin Pump or Continuous Glucose Monitor (CGM) Safely While You’re at MSK.
How to replace or remove your continuous glucose monitor
You can wear each sensor for 10 to 14 days, depending on which CGM system you have. Your CGM will send you an alert when it’s time to change your sensor.
To take off your sensor, pull the edge of the sticky area away from your skin. Use warm soapy water, adhesive removal, or alcohol to help take it off. Throw the used applicator and sensor away in a home medical sharps container. Read /node/20366 to learn more.
Put your new CGM in a different spot when replacing it to avoid irritating your skin. If your CGM goes into your arm, switch arms each time you replace it. If your CGM goes into your belly, put it in a different spot on your belly when you replace it.
Your care team will ask you to take off your device before some tests or procedures. Examples include magnetic resonance imaging (MRI) scans and computed tomography (CT) scans. Talk with your healthcare provider for more information.
When to call your healthcare provider
Call your diabetes healthcare provider if you have either of these:
- Hypoglycemia. This is blood glucose below 70 milligrams (mg) per decilitre (dL).
-
Hyperglycemia. This can be:
- More than 1 blood glucose reading above 200 mg/dL for 2 to 3 days in a row.
- Blood glucose above 300 mg/dL 2 times in 24 hours.
