This information describes fertility evaluation and fertility preservation options for people born with ovaries and a uterus. It’s meant for people who have finished cancer treatment. It explains:
- How cancer treatment may affect your fertility (ability to get pregnant).
- How your fertility can be evaluated after treatment.
- How you may be able to preserve your fertility after treatment.
In this resource, we use the word “female” to refer to people born with ovaries and a uterus.
Basic reproductive biology
Understanding basic reproductive biology can be helpful as you make decisions about your fertility. The female reproductive system has several parts that are explained in this section (see Figure 1).
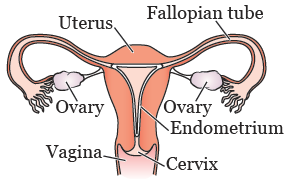
Figure 1. Female reproductive system
Ovulation
The ovaries have 2 functions:
- They produce hormones (estrogen and progestin).
- They hold your eggs (oocytes). Each egg is contained in a sac called a follicle.
When you start puberty, your pituitary gland (located in your brain) releases hormones that cause a group of follicles to grow each month. The egg inside each growing follicle starts to mature. As the follicles grow, the ovary releases hormones that cause the lining of your uterus (endometrium) to thicken and prepare for a pregnancy.
One egg from the group of growing follicles fully matures each month. It’s released from one of your ovaries into the fallopian tube. This process is called ovulation. The other follicles growing that month break down and the eggs are cleared from the body. Through this monthly process, females lose many eggs over time.
Pregnancy
If you’re not using birth control and you have vaginal sex with a male partner around the time you’re ovulating, a single sperm may fertilize the egg. The fertilized egg begins to divide, forming an embryo. If the embryo implants in the endometrium, you become pregnant. The cells of the embryo continue to divide, becoming a fetus. During pregnancy, your uterus expands to hold the fetus as it grows.
Menstruation
If the egg released during ovulation doesn’t become fertilized, or if the embryo doesn’t implant in the endometrium, hormone levels drop and cause the lining of the uterus to shed. This bloody discharge forms your monthly menstrual period. The cycle then begins again, with new eggs maturing each month.
Ovarian reserve
Females are born with about 1 million eggs. During a female’s lifetime, only 400 to 500 eggs are released during ovulation. The other eggs die naturally over time, so the number of eggs in the ovaries (called the ovarian reserve) gradually gets lower (see Figure 2). With fewer eggs, it’s harder to become pregnant. Eventually, there are so few eggs that a female becomes infertile (unable to get pregnant).
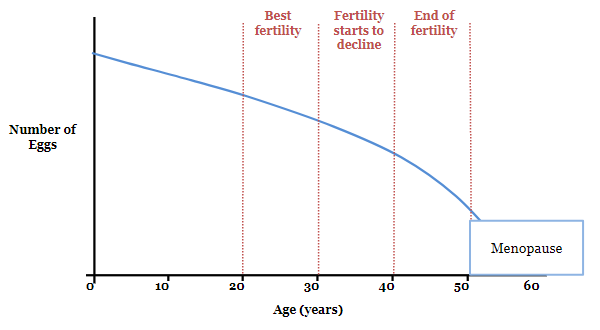
Figure 2. Ovarian reserve and age
Menopause
With the loss of eggs, the ovaries stop producing hormones. This causes monthly menstrual periods to stop. When a female’s menstrual periods stop, this is called menopause. Most females lose their fertility 5 to 10 years before menopause. This is because of both the loss of eggs and because the quality of their eggs declines over time.
Effects of cancer treatment on fertility
Cancer treatments can affect fertility in a number of ways.
-
Some chemotherapy medications destroy eggs. This decrease in the number of eggs may lead to infertility after treatment.
- The risk of infertility depends on the medications used, the doses given, and the age of the female at the time of treatment. Older females have fewer eggs when they start treatment. This means they are more likely to become infertile after treatment.
- This loss of eggs in the ovaries from chemotherapy can reduce the chance of pregnancy in the same way that natural aging does. Some females lose so many eggs that they become infertile and begin menopause immediately after treatment. Some females still have eggs remaining after treatment but may develop infertility and menopause at a young age. This narrows the window of time that a female can become pregnant.
-
Radiation therapy to the pelvis or whole abdomen (belly) destroys eggs in a similar way to chemotherapy. Radiation may also damage the uterus, causing fibrosis (scarring).
- Depending on the dose of radiation to the uterus, females may not be able to become pregnant after radiation. Females who do become pregnant may not be able to safely carry a pregnancy because their uterus may not be able to expand with a growing fetus. This can make you more likely to have a miscarriage or premature labor.
- Surgery or radiation therapy to the brain may affect the pituitary gland, which releases hormones that stimulate egg maturation and ovulation. However, this doesn’t damage the eggs in the ovaries, and medications that replace these hormones may allow the female to become pregnant.
- Surgery involving a single ovary, both ovaries, or the uterus can affect fertility.
Because of the many factors that can affect fertility, it’s hard to know how you may be affected by your treatment. We can’t know for sure who will still be able to get pregnant after treatment is finished and who will not. We also can’t know for sure how long a female will be fertile after treatment. If you have questions about your risk of infertility based on the treatment you received, speak with your oncologist (cancer doctor).
Fertility evaluation
Some females want to be evaluated after treatment to know their fertility status. This is done by a specially trained gynecologist, called a reproductive endocrinologist (RE). We don’t have REs at MSK, but we can make a referral for you.
We generally recommend that you wait at least 1 year after completing cancer treatment before having your fertility evaluated. This gives your ovaries time to recover from the effects of treatment.
The RE will do a number of tests to evaluate you. The tests may include:
- A transvaginal ultrasound, in which a thin wand is placed in your vagina. Sound waves from the wand create pictures of your ovaries and uterus. With this test, your doctor can examine your ovaries and count the number of large growing follicles in your ovaries. This is called the antral follicle count. If you’ve never had a gynecologic exam or vaginal sex, your RE may be able to perform the ultrasound using a wand placed on your abdomen rather than in your vagina.
- Blood tests to measure the levels of hormones related to fertility, including follicle stimulating hormone (FSH) and anti-mullerian hormone (AMH).
Your RE will review the results of the evaluation with you and discuss your options for preserving your fertility and building a family in the future.
If you have never had a gynecologic exam before, you may find it helpful to read Your First Gynecologic Visit by the American College of Obstetricians and Gynecologists before your appointment. You can search for it on www.acog.org.
Fertility preservation
Fertility preservation with egg freezing
Some females who are fertile after treatment, but are at risk of losing their fertility at a young age, may want to consider egg freezing. This involves removing mature eggs from your ovary to freeze and store for possible use in the future. The process generally takes about 2 weeks.
There are several steps involved in egg freezing, including:
-
Ovarian stimulation: On or around the second day of your period, you will start giving yourself hormone injections (shots) each day for about 10 days. A nurse at the fertility center will teach you how to do this. These hormones will stimulate multiple eggs in your ovaries to mature.
- During this period of stimulation, you will see the RE almost every other day for blood tests and ultrasounds. These tests show how your ovaries are responding to the hormones. Once your eggs are fully mature, the egg retrieval will be scheduled.
-
Egg retrieval: This is an outpatient procedure that’s done with anesthesia (medication to make you sleep), so you won’t feel any pain. You don’t need an incision (surgical cut).
- Once you’re asleep, an ultrasound wand is placed in your vagina so your RE can see your ovaries. A very thin needle is passed through the wall of your vagina up to your ovary to collect the mature eggs (see Figure 3).
- The entire procedure takes about 20 minutes and most females are discharged within 1 hour.
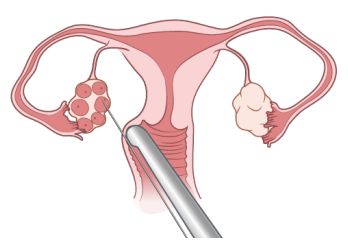
Figure 3. Egg retrieval
- Freezing (cryopreservation): After the eggs are collected, they are brought to the laboratory to be examined and processed. The following day, the eggs that have fully matured are frozen for your future use. They can be stored for as long as you want.
The more eggs you’re able to freeze, the greater the chance that you will be successful in having a baby using these eggs in the future. Depending on how many mature eggs you’re able to freeze, your RE may suggest you undergo a second cycle of stimulation and egg retrieval.
Fertility preservation with embryo freezing
Some females choose to freeze embryos rather than eggs. The process for embryo freezing and egg freezing are the same. However, after the egg retrieval, your eggs are fertilized with sperm from your male partner or from a sperm donor to create embryos. This is called in vitro fertilization (IVF).
Cost of egg and embryo freezing
Freezing eggs and embryos is costly, and unfortunately, many health insurance plans don’t cover the cost. This may change in the future. The cost is different from center to center. Some centers may offer a discount to those who were treated for cancer.
There are additional costs for the hormone medication needed for ovarian stimulation. If your prescription plan doesn’t cover these medications, LIVESTRONG Fertility may help:
-
LIVESTRONG Fertility works with a pharmaceutical company to provide free medication to people being treated at participating fertility centers. Eligibility is based on your income and not every fertility center participates.
- To learn more go to www.livestrong.org/we-can-help/livestrong-fertility
- To get an application, go to https://livestrongfertilityportal.unicentric.com/Login/Index#. You must submit the application and get approval before you start ovarian stimulation. To speak directly with one of their navigators, call 855-844-7777.
There will be an annual storage fee to keep your eggs or embryos frozen. There are also additional costs when you’re ready to thaw and use the eggs or embryos to attempt pregnancy. A financial specialist at the fertility center can check what will be covered by your health insurance and what you will have to pay yourself.
How frozen eggs and embryos are used to attempt pregnancy
If you use your frozen eggs or embryos in the future, they will be thawed when you’re ready to attempt pregnancy. If you froze eggs, they will be fertilized with sperm to create embryos.
If you no longer have regular periods, or are in menopause from your treatment, you will need to take hormones for several weeks to get the lining of your uterus ready for pregnancy. The embryos will be transferred into your uterus. The embryos are drawn up into a very thin, soft catheter that is passed through your vagina and cervix into your uterus. The embryos are released and the catheter is taken out. The procedure is done in an exam room. It does not hurt, so you will not need anesthesia. If you’re not able to carry a pregnancy yourself, they can be transferred to the uterus of another female to carry the pregnancy for you. This is called surrogacy with a gestational carrier.
About 2 weeks after the embryo transfer, a blood test is done to see if you, or your gestational carrier, have become pregnant. If the pregnancy test is positive, an ultrasound will be done several weeks later to see if the embryo has implanted to confirm the pregnancy. You will then schedule an appointment with an obstetrician (a doctor who specializes in pregnancy and childbirth) who will care for you during the pregnancy. You may need to continue taking hormones for several months to support the pregnancy.
If the embryo didn’t implant, and you have other embryos being stored, your RE can perform another embryo transfer when you’re ready.
Success rates with frozen eggs and embryos
The chance that you will be successful in having a baby using frozen eggs or embryos depends on your age at the time of egg retrieval and the number of mature eggs obtained from the procedure. Not every egg collected can become a baby. Some eggs won’t survive the freeze-thaw cycle. Some won’t fertilize and develop into embryos, and some may not implant after the transfer. Females under 35 years of age generally have a higher chance of success. Discuss your personal chance of success with your RE after your initial evaluation.
Other options for building a family
Some females will not be able to preserve their fertility after treatment and some may choose not to for personal reasons. If you’re unable to have a biological child in the future, there are other ways of building a family after cancer treatment.
- You can use donor eggs or embryos. Donor eggs are given by young females who undergo a cycle of ovarian stimulation and egg retrieval. These are fertilized with sperm from your partner or a donor to create embryos for transferred into your uterus. The cost of using donor eggs is about $35,000. Donor embryos are usually given by couples who had infertility treatment, have completed building their families, and do not want to discard their remaining embryos. The cost of using donor embryos is much lower than that of donor eggs.
- You can adopt. Having a history of cancer doesn’t prevent you from being able to adopt, as long as you’re now healthy and have been cancer-free for several years. Adopting a newborn baby in the United States costs about $30,000 to $40,000 and can take about 2 years.
To learn more about these options, read Building Your Family After Cancer Treatment: For People Born With Ovaries and a Uterus.
Making a decision about fertility preservation
It can be difficult to make a decision about fertility preservation because there is a lot of uncertainty. We can’t predict exactly how or if treatment will affect your fertility. If you do pursue fertility preservation, there are no guarantees that it will be successful.
There is no “right” decision. Our goal is for you to have all the information you need to make the best decision you can for yourself. Many females find it helpful to see a RE to be evaluated. Based on the results, the RE can discuss your risks, options, and chances of success in more detail to help you make a decision.
For more information, or to obtain a referral to a RE, ask your oncologist to refer you to one of our Fertility Nurse Specialists. Speaking with someone at our Counseling Center may also be helpful.
Questions to ask your doctor
If you have not discussed fertility with your doctor, you may find it helpful to ask some of the questions below:
- Have other females been able to get pregnant naturally after receiving the same treatment that I received?
- Will I be able to carry a pregnancy based on the treatment I received?
- Am I at risk for infertility or early menopause from the treatment I received?
- If I’m at risk for infertility or early menopause, but I’m not ready to have children yet, can I freeze eggs or embryos now to preserve my fertility for the future?
- If I carry a pregnancy, are there any risks to me or my baby based on the treatment I received?
- Are there any risks to the health of my children based on the type of cancer I had?
- Would a future pregnancy increase the chance of my cancer coming back?
- Are there specialists you can refer me to for help in addressing these issues?
