This information will help you get ready for your HDR brachytherapy (BRAY-kee-THAYR-uh-pee) treatment to your prostate at MSK.
Read through this resource at least once before your brachytherapy procedure. Use it as a reference in the days leading up to your treatment.
About your prostate
Your prostate is a small, firm gland about the size of a walnut. It works with other glands in your body to make semen.
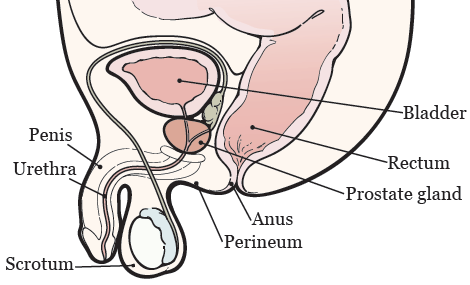
Figure 1. Your prostate anatomy
Your prostate is in front of your rectum, below your bladder (see Figure 1). It surrounds your urethra, the tube that drains urine (pee) from your bladder.
About HDR brachytherapy
Brachytherapy is a type of radiation therapy. Radiation therapy kills cancer cells by making it hard for them to multiply. In brachytherapy a radiation source is placed directly into or next to a tumor.
With HDR brachytherapy, your healthcare provider will place needles inside your prostate gland. These needles will be attached to tubes that will deliver the radiation source into your prostate. After your treatment, the tubes and needles will be removed.
There are 2 steps for your HDR treatment:
- You’ll have a procedure to place the needles into your prostate. This will be done under anesthesia, so you’ll be asleep.
-
You’ll have your HDR treatment(s), which are also called fractions.
- You may have 1 or 2 treatments. Your radiation oncologist will discuss this with you during your first visit with them.
- Your first treatment will be done in the operating room, right after your needle placement procedure. If you need a second treatment, it will be done exactly the same way on a different day.
- After treatment, the needles will be removed.
- You’ll go home the same day you have your treatments.
Your role on your radiation therapy team
You’ll have a team of healthcare providers working together to provide the right care for you. You’re part of the team, and your role includes:
- Arriving on time for your procedure.
- Asking questions and talking about your concerns.
- Telling someone on your radiation therapy team when you have side effects or pain.
-
Caring for yourself at home.
- Quitting smoking, if you smoke. If you want to quit, call our Tobacco Treatment Program at 212-610-0507.
- Drinking liquids as instructed.
- Eating the foods suggested by your radiation therapy team.
- Maintaining your weight.
Getting ready for your procedure
You and your care team will work together to get ready for your procedure. Help us keep you safe by telling us if any of these things apply to you, even if you’re not sure.
-
I take an anticoagulant (blood thinner), such as:These are examples of medicines. There are others.
Be sure your healthcare provider knows all the medicines you’re taking.- Aspirin
- Heparin
- Warfarin (Jantoven®, Coumadin®)
- Clopidogrel (Plavix®)
- Enoxaparin (Lovenox®)
- Dabigatran (Pradaxa®)
- Apixaban (Eliquis®)
- Rivaroxaban (Xarelto®)
-
I take an SGLT2 inhibitor, such as:
- Canagliflozin (Invokana®)
- Dapagliflozin (Farxiga®)
- Empagliflozin (Jardiance®)
- Ertugliflozin (Steglatro®)
- I take prescription medicine(s), including patches and creams. A prescription medicine is one you can only get with a prescription from your healthcare provider.
- I take over-the-counter medicine(s), including patches and creams. An over-the-counter medicine is one you can buy without a prescription.
- I take dietary supplements, such as herbs, vitamins, minerals, or natural or home remedies.
- I have a pacemaker, automatic implantable cardioverter-defibrillator (AICD), or other heart device.
- I have sleep apnea.
- I have had a problem with anesthesia (A-nes-THEE-zhuh) in the past. Anesthesia is medicine to you sleep during a surgery or procedure.
- I’m allergic to certain medicines or materials, including latex.
- I’m not willing to receive a blood transfusion.
- I drink alcohol.
- I smoke or use an electronic smoking device, such as a vape pen or e-cigarette.
- I use recreational drugs, such as marijuana.
Consider banking your sperm
For more information, read Sperm Banking and Building Your Family After Cancer Treatment: For People Born With Testicles.
Presurgical testing (PST)
You’ll have a PST appointment before your procedure. You’ll get a reminder from your healthcare provider’s office with the appointment date, time, and location. Visit www.msk.org/parking for parking information and directions to all MSK locations.
You can eat and take your usual medicines the day of your PST appointment.
It’s helpful to bring these things to your appointment:
- A list of all the medicines you’re taking, including prescription and over-the-counter medicines, patches, and creams.
- Results of any medical tests done outside of MSK in the past year, if you have them. Examples include results from a cardiac stress test, echocardiogram, or carotid doppler study.
- The names and telephone numbers of your healthcare providers.
You’ll meet with an advance practice provider (APP) during your PST appointment. They work closely with MSK’s anesthesiology (A-nes-THEE-zee-AH-loh-jee) staff. These are doctors with special training in using anesthesia during a procedure.
Your APP will review your medical and surgical history with you. You may have tests to plan your care, such as:
- An electrocardiogram (EKG) to check your heart rhythm.
- A chest X-ray.
- Blood tests.
Your APP may recommend you see other healthcare providers. They’ll also talk with you about which medicine(s) to take the morning of your procedure.
About drinking alcohol
It’s important to talk with your healthcare providers about how much alcohol you drink. This will help us plan your care.
If you drink alcohol regularly, you may be at risk for problems during and after your procedure. These include bleeding, infections, heart problems, and a longer hospital stay.
If you drink alcohol regularly and stop suddenly, it can cause seizures, delirium, and death. If we know you’re at risk for these problems, we can prescribe medications to help prevent them.
Here are things you can do before your procedure to keep from having problems.
- Be honest with your healthcare providers about how much alcohol you drink.
-
Try to stop drinking alcohol once your procedure is planned. Tell your healthcare provider right away if you:
- Get a headache.
- Feel nauseous (like you’re going to throw up).
- Feel more anxious (nervous or worried) than usual.
- Cannot sleep.
- Tell your healthcare provider if you cannot stop drinking.
- Ask your healthcare provider questions about drinking and procedures. All your medical information will be kept private, as always.
About smoking
If you smoke or use an electronic smoking device, you can have breathing problems when you have a procedure. Vapes and e-cigarettes are examples of electronic smoking devices. Stopping for even a few days before your procedure can help prevent breathing problems during and after your procedure.
Your healthcare provider will refer you to our Tobacco Treatment Program if you smoke. You can also reach the program by calling 212-610-0507.
About sleep apnea
Sleep apnea is a common breathing problem. If you have sleep apnea, you stop breathing for short lengths of time while you’re asleep. The most common type is obstructive sleep apnea (OSA). With OSA, your airway becomes fully blocked during sleep.
OSA can cause serious problems during and after a procedure. Tell us if you have or think you might have sleep apnea. If you use a breathing device, such as a CPAP machine, bring it on the day of your procedure.
Arrange for someone to take you home
You must have a responsible care partner take you home after your procedure. A responsible care partner is someone who can help you get home safely. They should be able to contact your care team if they have any concerns. Make sure to plan this before the day of your procedure.
If you don’t have a responsible care partner to take you home, call one of the agencies below. They’ll send someone to go home with you. There’s a charge for this service, and you’ll need to provide transportation. It’s OK to use a taxi or car service, but you still need a responsible care partner with you.
| Agencies in New York | Agencies in New Jersey |
| VNS Health: 888-735-8913 | Caring People: 877-227-4649 |
| Caring People: 877-227-4649 |
We recommend you have someone to help at home for the first 24 hours after your procedure.
Fill out a Health Care Proxy form
If you have not already filled out a Health Care Proxy form, we recommend you do now. If you already filled one out or have any other advance directives, bring them to your next appointment.
A health care proxy is a legal document. It says who will speak for you if you cannot communicate for yourself. This person is called your health care agent.
- To learn about health care proxies and other advance directives, read Advance Care Planning for People With Cancer and Their Loved Ones.
- To learn about being a health care agent, read How to Be a Health Care Agent.
Talk with a member of your care team if you have questions about filling out a Health Care Proxy form.
Do physical activity
Doing physical activity will help your body get into its best condition for your procedure. It will also make your recovery faster and easier.
Try to do physical activity every day. Any activity that makes your heart beat faster, such as walking, swimming, or biking, is a good choice. If it’s cold outside, use stairs in your home or go to a mall or shopping center
Follow a healthy diet
Follow a well-balanced, healthy diet before your procedure. If you need help with your diet, talk with your healthcare provider about meeting with a clinical dietitian nutritionist.
Buy your supplies
Buy the bowel preparation kit your healthcare provider told you to use if you haven’t already done so.
- Bisacodyl (Dulcolax®) 5 milligram (mg) tablets. These are usually sold as a box of 10 tablets, but you’ll only need to take 1 tablet.
- NuLYTELY® solution and flavor packs (cherry, lemon-lime, orange, and pineapple). This comes in a 1-gallon (128-ounce) bottle, but you’ll only need to drink ½ gallon (64 ounces). Your healthcare provider will give you a prescription for this.
This is also a good time to stock up on clear liquids to drink the day before your procedure. Read the table in the “Follow a Clear Liquid Diet” section for examples of liquids to buy.
7 days before your procedure
Follow your healthcare provider’s instructions for taking aspirin
Aspirin can cause bleeding. If you take aspirin or a medicine that has aspirin, you may need to change your dose or stop taking it 7 days before your procedure. Follow your healthcare provider’s instructions. Do not stop taking aspirin unless they tell you to.
To learn more, read How To Check if a Medicine or Supplement Has Aspirin, Other NSAIDs, Vitamin E, or Fish Oil.
Stop taking vitamin E, multivitamins, herbal remedies, and other dietary supplements
Vitamin E, multivitamins, herbal remedies, and other dietary supplements can cause bleeding. Stop taking them 7 days before your procedure. If your healthcare provider gives you other instructions, follow those instead.
To learn more, read Herbal Remedies and Cancer Treatment.
2 days before your procedure
Stop taking nonsteroidal anti-inflammatory drugs (NSAIDs)
NSAIDs, such as ibuprofen (Advil® and Motrin®) and naproxen (Aleve®), can cause bleeding. Stop taking them 2 days before your procedure. If your healthcare provider gives you other instructions, follow those instead.
To learn more, read How To Check if a Medicine or Supplement Has Aspirin, Other NSAIDs, Vitamin E, or Fish Oil.
1 day before your procedure
Note the time of your procedure
A staff member will call you after the day before your procedure. If your procedure is scheduled for a Monday, they’ll call you on the Friday before. If you do not get a call by , call 212-639-5014.
The staff member will tell you what time to arrive for your procedure. They’ll also remind you where to go.
This will be:
Memorial Hospital (MSK’s main hospital)
1275 York Ave. (between East 67th and East 68th streets)
New York, NY 10065
Visit www.msk.org/parking for parking information and directions to all MSK locations.
If you have any changes in your health or need to cancel your procedure for any reason, call your radiation oncologist.
Prepare your NuLYTELY bowel preparation solution
On the morning of the day before your procedure, add lukewarm water to the NuLYTELY, filling it to the top of the line on the bottle. Add a flavor pack, if you choose. Use only a flavor pack that was provided with your NuLYTELY.
With the cap on, shake the NuLYTELY bottle until the powder is dissolved. The mixture will be clear, even if you used a flavor pack. If you prefer, you can place the bottle in the refrigerator to chill it. Many people have told us that NuLYTELY tastes better cold. Don’t mix the NuLYTELY earlier than the morning before your procedure.
Follow a clear liquid diet
- You can have solid food for breakfast and lunch. Aim to finish your lunch by 12 p.m. (noon).
-
After lunch, start the clear liquid diet.
- A clear liquid diet includes only liquids you can see through. Examples are listed in the “Clear Liquid Diet” table.
- Try to drink at least 1 (8-ounce) cup of clear liquid every hour while you’re awake.
- Drink different types of clear liquids. Do not just drink water, coffee, and tea.
- Do not drink more than 2 cups (16 ounces) of liquids with caffeine.
- Do not drink diet liquids, even if you have diabetes. If you do, you may feel weak or dizzy.
| Clear liquid diet | ||
|---|---|---|
| OK to have | Do not have | |
| Soups |
|
|
| Sweets |
|
|
| Drinks |
|
|
Take a bisacodyl tablet
At on the day before your procedure, swallow 1 bisacodyl tablet with water.
Drink the NyLYTELY bowel preparation
At on the day before your procedure, start drinking the NuLYTELY. Drink 1 (8-ounce) cup of the mixture every 15 minutes. Drink only half of the NuLYTELY solution (64 ounces). Throw out the other half. Then, keep drinking clear liquids.
The NuLYTELY will cause frequent bowel movements, so be sure to be near a bathroom when you start drinking it. To help prevent irritation, you can apply petroleum jelly (Vaseline®) or A&D® ointment to the skin around your anus after every bowel movement.
The night before your procedure
- Take the medications your healthcare provider told you to take the night before your procedure. Take them with a small sip of water.
- Shower using soap and water the night before or the morning of your procedure.
Instructions for eating
Stop eating at midnight (12 a.m.) the night before your procedure. This includes hard candy and gum.
Your healthcare provider may have given you different instructions for when to stop eating. If so, follow their instructions. Some people need to fast (not eat) for longer before their procedure.
The day of your procedure
Instructions for drinking
Between midnight (12 a.m.) and 2 hours before your arrival time, only drink the liquids on the list below. Do not eat or drink anything else. Stop drinking 2 hours before your arrival time.
- Water.
- Clear apple juice, clear grape juice, or clear cranberry juice.
- Gatorade or Powerade.
-
Black coffee or plain tea. It’s OK to add sugar. Do not add anything else.
- Do not add any amount of any type of milk or creamer. This includes plant-based milks and creamers.
- Do not add honey.
- Do not add flavored syrup.
If you have diabetes, pay attention to the amount of sugar in your drinks. It will be easier to control your blood sugar levels if you include sugar-free, low-sugar, or no added sugar versions of these drinks.
It’s helpful to stay hydrated before procedures, so drink if you are thirsty. Do not drink more than you need. You will get intravenous (IV) fluids during your procedure.
Stop drinking 2 hours before your arrival time. This includes water.
Your healthcare provider may have given you different instructions for when to stop drinking. If so, follow their instructions.
Take your medications as instructed
Take the medications your healthcare provider told you to take the morning of your procedure. Take them with a small sip of water.
Things to remember
- If you did not shower the night before your procedure, take a shower the morning of your procedure.
- Don’t put on any lotion, cream, deodorant, powder, or cologne.
- Wear loose-fitting, comfortable clothes.
- Don’t wear any metal objects. Remove all jewelry, including body piercings. The equipment used during your procedure can cause burns if it touches metal.
- Leave valuable items (such as credit cards, jewelry, and your checkbook) at home.
- If you wear contact lenses, wear your glasses instead. If you don’t have glasses, bring a case for your contacts.
Once you’re in the hospital
When you get to the hospital, take the B elevator to the 6th floor. Check in at the desk in the PSC waiting room.
Many staff members will ask you to say and spell your name and birth date. This is for your safety. People with the same or a similar name may be having a procedure on the same day.
When it’s time to change for your procedure, you’ll get a hospital gown, robe, and nonskid socks to wear.
Meet with a nurse
You’ll meet with a nurse before your procedure. Tell them the dose of any medications you took after midnight and the time you took them. Make sure to include prescription and over-the-counter medications, patches, and creams. Tell your nurse if you’re wearing dentures or hearing aids. You will need to take them out before your procedure.
Your nurse may place an intravenous (IV) line in one of your veins, usually in your arm or hand. If your nurse does not place the IV, your anesthesiologist will do it in the procedure room.
During your procedure
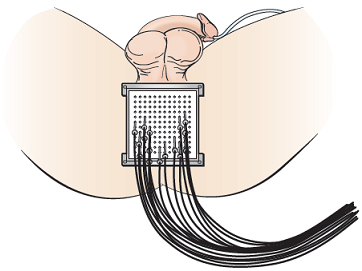
Figure 2. Template with catheters
When it’s time for your procedure, you’ll either walk into the operating room or be taken in on a stretcher. A member of the operating room team will help you onto the operating bed. Compression boots will be placed on your lower legs. These gently inflate and deflate to help blood flow in your legs.
Once you’re comfortable, your anesthesiologist will give you anesthesia through your IV line and you’ll fall asleep. You’ll also get fluids through your IV line during and after your procedure.
After you’re fully asleep, a breathing tube will be placed through your mouth and into your windpipe to help you breathe. A urinary (Foley) catheter will also be placed to drain urine from your bladder.
After the Foley catheter is in place, your healthcare provider will use a rectal ultrasound to see your prostate. They’ll put 12 to 22 tiny needles into your prostate through your perineum (the area of skin between your scrotum and anus). The needles are guided to the exact locations in and around your prostate through a square metal template. The template will be positioned up against your perineum (see Figure 2).
During your treatment
For your treatment, tubes will be connected to the needles in your prostate to deliver the radiation. The tubes look like long, plastic straws (see Figure 2). The cables are connected to a machine that stores the radioactive source (Iridium-192).
After the right amount of radiation is delivered to your prostate, the tubes will be disconnected and the treatment will end.
The needles will be removed from your prostate after the treatment is finished. Your nurse will apply pressure and an ice pack to your perineum to help with any bleeding. The Foley catheter and breathing tube will be removed before you wake up from anesthesia.
After your procedure
In the hospital
You’ll wake up in the Post-Anesthesia Care Unit (PACU). A nurse will be keeping track of your temperature, pulse, blood pressure, and oxygen levels. In rare cases, you may still have a Foley catheter in your bladder to keep track of how much urine you’re making.
You may have some pain after your procedure. Your healthcare providers will ask you about your pain often. You’ll be given medication to treat your pain as needed. If your pain isn’t relieved, please tell one of your healthcare providers.
Most people go home on the same day as their procedure and treatment. After your catheter is removed, you’ll need to urinate on your own before you can go home.
After your treatment is finished, you aren’t radioactive and don’t need to follow any radiation precautions.
At home
Medications
- Radiation to the prostate often causes urinary frequency and urgency (feeling that you need to urinate more often or very suddenly). To manage these side effects, keep taking all urinary medications as prescribed, such as tamsulosin (Flomax®), silodosin (Rapaflo®), or alfuzosin (Uroxatral®). Tell your healthcare provider if you don’t have these medications at home.
- After your procedure, you may feel burning when you urinate. This is from the Foley catheter that was placed in your bladder. You’ll get a prescription for medication to help with the burning called phenazopyridine (Pyridium®).
Other instructions
- Rarely, you may have some bleeding in your perineum where the needles entered. If this happens, apply steady pressure with a clean, dry washcloth or gauze for 5 minutes. If the bleeding becomes heavy or doesn’t stop, call your healthcare provider.
- You can resume your regular diet. You may want avoid things that may irritate your bladder. These include caffeine (such as coffee and tea), alcohol, citrus juices, and spicy foods.
- You can shower after you’re discharged from the hospital.
- Don’t lift anything over 20 pounds (9.1 kilograms) for at least 1 week after your procedure.
- Most people can go back to work 2 days after their procedure. If your job requires heavy lifting, ask your healthcare provider when you can go back to work.
Side effects
Urinary symptoms
Urinary symptoms are the most common side effects of brachytherapy. After your procedure, you may have some of the following symptoms.
- Some people can’t urinate after the procedure or may only be able to urinate a few drops at a time. This is an emergency. Call your healthcare provider right away if you can’t urinate.
- You may need to urinate more often than usual, as many as 1 or more times an hour. This usually starts 2 to 4 weeks after your procedure and can last several months or longer.
- You may have some burning during urination. This usually starts 2 to 4 weeks after your procedure and can last for about 4 to 12 months.
- You may notice blood in your urine, which will make it look pink. This is common and usually disappears 3 to 7 days after your procedure. Call your healthcare provider if bleeding continues after 7 days or if you pass blood clots in your urine.
- You may have bruising and or swelling around your scrotum, testicles, and penis. This should go away 1 to 2 weeks after your procedure. Call your healthcare provider if you still have bruising after 2 weeks.
Talk with your healthcare provider if you have any of these symptoms. If you have a procedure to look at your bladder (such as a cystoscopy) planned, wait to have it until after you’ve talked with your healthcare provider.
Pain
You may have some mild pain for 1 or 2 days after your procedure. You can take an over-the-counter pain medication such as acetaminophen (Tylenol®), ibuprofen (Advil®), or naproxen (Aleve®) to help with pain. If these doesn’t help your pain, call your healthcare provider.
Sexual health
You may have concerns about the effects of cancer and your treatment on your sexuality. After your treatment, you aren’t radioactive. You can’t pass radiation to anyone else, so it’s safe to be in close contact with other people.
You can be sexually active after your HDR brachytherapy treatment unless your radiation oncologist gives you other instructions. However, if you’re sexually active with a woman who can have children, you must use birth control (contraception) to prevent pregnancy during your entire prostate cancer treatment. You must keep using birth control for 1 year after your treatment is finished. This is to make sure you don’t conceive with sperm that may have been damaged by exposure to radiation, which could possibly result in birth defects.
You may have temporary or permanent numbness in the head of your penis, although this is rare.
You may also develop sexual changes after your treatment. You may have:
- Erectile dysfunction (difficultly or inability to have or maintain an erection).
- A change in the sensation of orgasm.
- A change in the amount or consistency of your ejaculation.
These sexual changes may occur many months or even years after treatment.
There are treatments for erectile dysfunction. MSK has a Male Sexual and Reproductive Medicine Program to help people address the impact of their disease and treatment on their sexual health. You can meet with a specialist before, during, or after your treatment. Your healthcare provider can give you a referral, or you can call 646-888-6024 for an appointment.
An excellent resource that discusses sexual health issues during treatment is the booklet Sex and the Man With Cancer. You can get a copy of this booklet from the American Cancer Society by calling 800-227-2345 or by searching for it at www.cancer.org.
Support services
MSK support services
Visit the Cancer Types section of MSK’s website at www.msk.org/types for more information.
Admitting Office
212-639-7606
Call if you have questions about your hospital admission, such as asking for a private room.
Anesthesia
212-639-6840
Call if you have questions about anesthesia.
Integrative Medicine Service
www.msk.org/integrativemedicine
Our Integrative Medicine Service offers many services to complement (go along with) traditional medical care, including music therapy, mind/body therapies, dance and movement therapy, yoga, and touch therapy. To schedule an appointment for these services, call 646-449-1010.
You can also schedule a consultation with a healthcare provider in the Integrative Medicine Service. They will work with you to come up with a plan for creating a healthy lifestyle and managing side effects. To make an appointment, call 646-608-8550.
Male Sexual and Reproductive Medicine Program
646-888-6024
Cancer and cancer treatments can affect your sexual health, fertility, or both. Our Male Sexual and Reproductive Medicine Program can help with sexual health problems, such as erectile dysfunction (ED). We can help before, during, or after your treatment. Call for more information or to make an appointment.
Nutrition Services
www.msk.org/nutrition
212-639-7312
Our Nutrition Service offers nutritional counseling with one of our clinical dietitian-nutritionists. Your clinical dietitian-nutritionist will talk with you about your eating habits. They can also give advice on what to eat during and after treatment. To make an appointment, ask a member of your care team for a referral or call the number above.
Patient and Caregiver Education
www.msk.org/pe
Visit our Patient and Caregiver Education website to search for educational resources, videos, and online programs.
Patient Billing
646-227-3378
Call if you have questions about preauthorization with your insurance company. This is also called preapproval.
Patient Representative Office
212-639-7202
Call if you have questions about the Health Care Proxy form or concerns about your care.
Perioperative Nurse Liaison
212-639-5935
Call if you have questions about MSK releasing any information while you’re having surgery.
Private Duty Nurses and Companions
917-862-6373
You can request private nurses or companions to care for you in the hospital and at home. Call for more information.
When to call your healthcare provider
Call your healthcare provider if you have:
- New or worsening urinary symptoms.
- Difficulty urinating.
- Blood clots in your urine.
- A fever of 100.4 °F (38 °C) or higher.
- Pain that doesn’t get better after taking pain medication.