Chief of the Dermatology Service Allan Halpern, pictured here with nurse Nancy Eastman, has pioneered the use of whole-body photography for early detection and prevention of melanoma.
Our specialists use a few different methods to treat skin melanoma, depending on whether it has metastasized (spread) to other parts of your body or whether it’s contained within one tumor. Your options could include surgery, radiation therapy, or certain types of drugs. Your care team at MSK will come up with a personalized treatment plan that’s designed especially for your disease.
Surgery
Surgery is often the best option to cure melanoma that isn’t metastatic — and it also can be the only treatment you need to be rid of the disease.
Because melanoma cells can spread to other parts of the body, it’s important that we check whether this has happened when you have your surgery. To make sure we’ve eliminated all of the affected cells, our surgeons remove the tumor as well as some of the normal skin around it, called the tumor margins.
The amount we remove depends primarily on these factors:
- how thick the tumor is
- where it’s located on your body
- how removing the tumor might affect your appearance
Sometimes we recommend doing a skin graft, which is a minor procedure that involves removing a patch of skin from another part of your body to replace the tissue we remove.
If we determine that your tumor is likely to spread, we perform our most sensitive staging method — called sentinel lymph node biopsy — at the same time that we remove the melanoma.
For this procedure, we assess which lymph node the cancer cells are most likely to spread to first (the sentinel node) and remove it during surgery. Our pathologist examines the node very carefully to determine whether cancer cells are present. If they are, the surgeon may remove additional lymph nodes. If no cancer cells are present, we don’t recommend any further surgery.
Radiation Therapy for Local Melanoma
Sometimes we recommend radiation therapy for the area where the surgery was performed. The decision can be complicated, though. For some people, this approach may reduce the chances that melanoma comes back in that specific spot, but it doesn’t guarantee that melanoma won’t recur in other parts of your body.
And because radiation therapy can also cause side effects, our radiation oncologists are studying new ways of delivering it for people with melanoma, such as through intensity-modulated radiation therapy, a technique pioneered at MSK. By delivering radiation with this more precise and focused technique, it may be possible to avoid healthy, normal organs and prevent side effects.
We’re also currently the only center in North America participating in an international research study to determine if this approach helps prevent recurrence of melanoma in the head and neck area.
Radiation Therapy for Metastatic Melanoma
With radiation therapy, we can provide focused treatment to areas that are difficult to reach by surgery or other means. For example, if you have melanoma that has spread to the brain, we may treat the tumor with stereotactic radiosurgery, a procedure that enables us to deliver a single high dose of radiation directly to the tumor. This approach can eliminate the tumor with few side effects.
IMRT can also be combined with new image-guidance technology, a precise delivery process that’s more effective at controlling melanoma than other forms of radiation therapy.
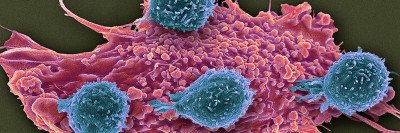
Immunotherapy for Metastatic Melanoma
Back in 2004, our patients were among the first to receive an immunotherapy drug called ipilimumab (Yervoy®), which activates the immune system to fight melanoma. We led studies showing that ipilimumab could prolong the overall survival of people with metastatic melanoma. The FDA approved the drug for general use in 2011 — seven years after it was first available to people being cared for at MSK.
Ipilimumab — which blocks an immune molecule called CTLA-4 — was a huge advance for patients with advanced melanoma, but even greater success has been achieved with another class of immunotherapy drugs that target PD-1, such as nivolumab (Opdivo®) and pembrolizumab (Keytruda®). Patients have been able to participate in clinical trials of these drugs since 2010, approximately four years before the FDA approved both drugs to treat melanoma in 2014.
To further improve upon ipilimumab and PD-1 blockers given individually, MSK has led clinical trials testing the combination of ipilimumab and nivolumab. We were the first center to test this combination in patients, and we led the large phase II and III clinical trials that led the FDA to approve this combination in 2015.
As we continue to pursue new melanoma drugs, many of our patients still choose to enroll in clinical trials, in many cases allowing them to access drugs still unavailable at most other places years before the FDA approves them for general use.
Targeted Therapy for Metastatic Melanoma
The DNA of melanoma usually contains many mutations. These are changes in the DNA sequence that are different from a person’s normal DNA. Some of these mutations are called driver mutations because they cause melanoma to grow continuously and ignore the usual “stop” signals sensed by normal cells. In about 40 percent of melanomas, the driver mutation is in a gene called BRAF. This mutation results in what is in essence a broken “on” switch.
MSK conducted the first-in-humans trial of a RAF inhibitor called vemurafenib (Zelboraf®) in 2006. Now, vemurafenib and another RAF inhibitor called dabrafenib (Taflinar™) are FDA approved. Both drugs can turn melanoma cells “off” if they have a BRAF mutation. When used in combination with another type of drug called a MEK inhibitor, this treatment can shrink melanomas in almost 70 percent of patients. One of the challenges is that the melanoma often becomes resistant to this treatment, but MSK scientists are working on methods to prevent this.
There are driver mutations in other genes besides BRAF. We are able to screen for mutations in more than 400 genes in melanoma tumors and are working to develop new treatments to target other common driver mutations.
Chemotherapy for Metastatic Melanoma
Although it’s much less commonly used than it once was, chemotherapy remains the best treatment option for some people. Some chemotherapy produces only mild side effects, but others can cause fatigue and loss of appetite that make it more difficult for you to carry on with your normal activities.
If you have melanoma confined to a single arm or leg, we can give chemotherapy medicines to the limb through an IV in a procedure called regional infusion therapy. This approach exposes the cancer to very high levels of chemotherapy while the rest of your body is spared, maximizing the drug’s effect while limiting its impact on the rest of your body. MSK doctors were among the first to use this technique, and through clinical trials, we’re actively investigating ways to make it even more effective.
Your MSK Follow-Up Providers
We’re available 24 hours a day, 7 days a week