What Is Cushing’s Disease?
Cushing’s disease occurs when a tumor arises in the corticotropic cells of the pituitary gland and begins to secrete a hormone called adrenocorticotropic hormone. Also called ACTH, this hormone, in turn, triggers the adrenal glands to produce the “stress hormone” known as cortisol.
Cortisol affects metabolism and under normal circumstances helps the body recover from stress caused by surgery, an injury, or an infection. When the body produces too much cortisol, it leads to a range of symptoms.
What Causes Cushing’s Disease?
The exact cause of ACTH-secreting tumors is unknown. Women in their 30s and 40s are most commonly diagnosed with the condition, although men and women of all ages can be affected.
Most ACTH-secreting tumors are benign (not cancer), though in rare cases, they can become cancerous.
Cushing’s Disease Signs & Symptoms
The most common symptoms of Cushing’s disease are:
- unexplained weight gain, particularly around the neck and midsection,
- thinning of the arms and legs and muscle weakness,
- diabetes,
- high blood pressure,
- easy bruising,
- moodiness or depression,
- insomnia and poor concentration,
- irregular or absent menstrual periods in women, and
- weakening of the bones and fractures.
Cushing’s Disease vs. Cushing’s Syndrome
Cushing’s syndrome, also called hypercortisolism, refers to the presence of excessive amounts of cortisol in the bloodstream over a lengthy period of time. The most common cause is steroid use. Other causes include ectopic tumors and adrenal cortex tumors.
Cushing’s disease refers only to hypercortisolism caused by the presence of a tumor in the pituitary gland.
Diagnosing Cushing’s Disease
Cushing’s disease is diagnosed using blood, urine, and saliva tests that look for abnormal amounts of the hormone cortisol.
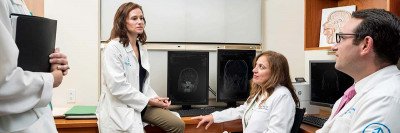
You may also need to have an MRI scan of the brain, where the pituitary gland is located, to determine the exact size and location of the tumor.
Cushing’s disease is not always easy to diagnose since there are a number of other conditions that can raise the levels of cortisol in the body. Sometimes your doctor may not have a clear diagnosis even after performing the standard blood test and an MRI.
At Memorial Sloan Kettering, your care team will run a variety of tests to rule out other conditions. If your initial results do not confirm a Cushing’s disease diagnosis, we may use a test called petrosal venous sampling.
Petrosal Venous Sampling to Diagnose Cushing’s Disease
Petrosal venous sampling is a minimally invasive procedure in which a doctor uses a special catheter to obtain a blood sample from the petrosal sinuses (the veins that drain the pituitary gland on both sides of the skull). This sample is then compared to a sample of blood taken from veins in the groin area to identify whether the pituitary gland is the source of excess ACTH.
An anesthesiologist administers sedation during the procedure. Patients typically do not experience any pain.
At Memorial Sloan Kettering, petrosal venous sampling is performed by an interventional radiologist with extensive experience in this procedure. State-of-the-art imaging (fluoroscopy and CT guidance) allows us to accurately and efficiently target the petrosal sinuses. Experience and precision are particularly important when conducting petrosal venous sampling to help avoid complications or the need for a second procedure.
If a tumor is present in the pituitary gland, the results will show higher levels of ACTH in the petrosal sample only. If a tumor located elsewhere in the body is raising the level of ACTH in the body, then the ACTH levels will be high but around the same level in both samples.
Interventional radiologists are doctors who use medical imaging, coupled with tools such as catheters and needles, to see inside the body, allowing them to address a large range of medical conditions that would have required surgery in the past. The interventional radiologists at MSK perform more than 14,000 procedures each year and are among the most experienced interventional radiology teams in the county.
Treatment Options for Cushing’s Disease
Cushing’s Disease Surgery to Remove Tumor
The primary treatment for Cushing’s disease is surgery to remove the pituitary tumor.
Memorial Sloan Kettering surgeons are experienced in using a minimally invasive approach called transsphenoidal surgery to remove pituitary tumors. The approach allows our surgeons to bypass brain tissue, operating instead through an incision inside the nasal passage. The risk for neurologic complications with this technique is very low, and the surgery leaves no visible scar.
In the rare case that a tumor is too large to be removed with transsphenoidal surgery, our surgeons may recommend a craniotomy, a procedure in which the tumor is removed through an incision made in the front of the skull.
Sometimes large ACTH-secreting tumors (macroadenomas) can be difficult to cure with surgery alone and may require additional therapy, such as radiation therapy or certain medications.
Radiation Therapy for Cushing’s Disease
Radiation therapy can be used in one of several ways for Cushing’s disease. It may be recommended as additional therapy after surgery to prevent regrowth of the tumor. Radiation may also be used as the sole treatment if the tumor cannot be removed surgically, or if the tumor regrows after surgery.
The radiation therapy team at MSK is highly experienced in caring for people with Cushing’s disease, and works closely with the other members of your care team. They have access to every form of modern radiation therapy available and will customize a treatment plan so precise that it factors in the size and shape of your tumor to the millimeter.
Their goal is to not only eliminate the tumor cells but to prevent the side effects of treatment by keeping the healthy cells around the tumor safe.
We offer several radiation therapy options for people with Cushing’s disease. Learn more about our approach to radiation therapy for pituitary tumors.
Medications for Cushing’s Disease
While surgery is usually the primary treatment for patients with Cushing’s disease, medications are needed in cases where there is persistent or recurrent disease after surgery, or in the rare case that surgery is not recommended. As there are currently only two FDA-approved medical therapies for Cushing’s disease, our doctors are currently exploring the use of new medications for Cushing’s in clinical trials (research studies that test new treatments to see how well they work).
See a list of available clinical trials for Cushing’s disease.
Support Services
Even after you’ve finished your primary treatments for Cushing’s Disease, you may still need our help. We’re committed to supporting you in every way we can — physically, emotionally, spiritually, and otherwise — for as long as you need us.
Learn more about ways we can help.
Sometimes, you and your loved ones just need someone to talk to, someone who’s trained to help you make sense of your experience before, during, and after treatment.
Our Counseling Center offers both individual and group counseling sessions to help you and your family cope with Cushing’s disease. These sessions can be a healthy, productive way to work through the stress and anxiety that are sometimes a part of treatment and recovery.
Learn more about how we can support your emotional well-being.
Medical treatments are generally the best way to treat your disease. Their whole purpose is to get you healthy again. But at MSK, we know that complementary services can also help soothe and heal not only your body but also your mind and spirit.
Our Integrative Medicine Service can be a valuable part of your formal treatment plan. Programs we offer include massage, acupuncture, hypnotherapy, meditation, visualization, music therapy, and nutritional counseling. Formal classes include yoga, tai chi, and chair aerobics.
Learn more about the variety of complementary services we offer.
Many people with Cushing’s disease have questions about diet and nutrition. Our food and nutrition team is trained in helping you understand and cope with the issues you may be facing.
Our expert dietitians provide medical nutrition therapy that can help you manage your weight and cope with other dietary issues. They’ll work closely with your treatment team to customize a nutrition plan that fits your own specific needs.
Learn more about our nutrition services for patients and survivors.
We understand that the side effects of cancer treatment that affect your physical appearance can be as upsetting and uncomfortable as any other symptoms you may have. Our dermatology experts can help you manage conditions that affect the health and appearance of your skin and, in some instances, even help prevent them from developing in the first place.
Learn more about how we can help you keep your skin healthy.
Monday through Friday, to (Eastern time)