Older, vulnerable patients with relapsed/refractory large B cell lymphoma (LBCL) should receive the same consideration for chimeric antigen receptor (CAR) T cell therapy as younger patients, according to our study published recently online and ahead of print in the journal Haematologica.
Among 49 patients who received CAR T at Memorial Sloan Kettering Cancer Center between January 2018 and March 2019, we found no significant differences in progression-free survival (PFS) or postrelapse overall survival (PR-OS) in those older than age 65 compared to those under 65. High-grade toxicities were not excessive and were similar in both groups. There were no significant differences between the age groups with respect to functional limitation, cognition, or comorbidity burden. (1)
Overall, our findings indicate that we should not automatically exclude older patients from consideration for CAR T based solely on chronological age, multiple morbidities, functional limitation, or cognitive impairment. Individualized care plans should also include attention to nononcologic geriatric issues.
These findings are important given that the Centers for Medicare and Medicaid Services has recently proposed complete coverage for CAR T for Medicare beneficiaries, in recognition of the significant need to improve outcomes among older patients with geriatric vulnerabilities. Our insights extend learning beyond the previously published results for older patients in the ZUMA-1 (2) and JULIET (3) trials and represent an entry point for a larger-scale investigation of geriatric vulnerabilities in CAR T.
At MSK, we continue to investigate the impact and safety of CAR T in expanded patient populations. We are participating in multicenter, collaborative, and registry studies that aim to prospectively identify geriatric impairments and validate the prognostic impact of CAR T in older patients. We are also developing a proper selection algorithm for older patients.
Relapsed/Refractory LBCL in Geriatric Patients
LBCL predominantly affects older adults and typically results in suboptimal outcomes, even when we treat patients with curative intent. (4) For patients with relapsed/refractory LBCL, outcomes are dismal and remain an unmet clinical need. (5)
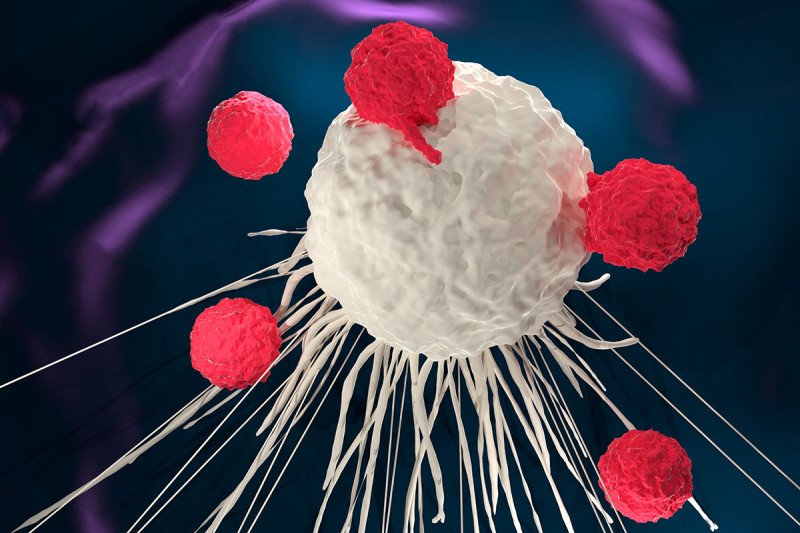
MSK scientists pioneered CAR T, which involves reengineering a patient’s immune cells to arm them with proteins that recognize cancer and infusing them back into the patient in large numbers. To date, the US Food and Drug Administration has approved two CAR T products: tisagenlecleucel in August 2017, for treating pediatric and young adult patients with a form of acute lymphoblastic leukemia; and axicabtagene ciloleucel in October 2017, for treating relapsed/refractory LBCL.
CAR T has revolutionized the treatment of patients with relapsed/refractory LBCL. (6) However, its impact and safety in vulnerable older patients, especially those with multiple morbidities and functional limitations, have not been reported. Geriatric vulnerabilities have been associated with poor survival and treatment-related toxicities in older patients with lymphoma who received anthracycline-based chemoimmunotherapy. (4)
CAR T versus Salvage Chemotherapy or Supportive Care in Older Patients
First, we analyzed outcomes for 42 consecutive patients age 65 or older with relapsed/ refractory LBCL and geriatric vulnerabilities who were referred for CAR T. A total of 24 patients received CAR T between January 2018 and March 2019. The remaining 18 patients did not meet the clinical eligibility requirements for CAR T and received salvage chemotherapy or supportive care instead. The two groups were comparable for age, gender, prior lines of therapy, relapse stage, comorbidity burden, and Karnofsky Performance Status. (1)
Not surprisingly, the patients who received CAR T had a significantly reduced risk of death compared to those who did not receive CAR T, with a hazard ratio (HR) of 0.31 (95 percent CI: 0.10 to 0.93, p=0.04) at a median follow-up of 291 days (range: 162 to 572) for survivors. Selection bias for patients who did not have rapidly progressing disease, significant comorbidities, or suboptimal performance status likely played a role in these results. (1)
CAR T in Older versus Younger Patients
Next, we compared the outcomes for the group of 24 patients age 65 or older who received CAR T with those from an additional cohort of 25 patients under age 65 who received CAR T for relapsed/refractory LBCL during the same period. (1)
All of these 49 patients met the eligibility criteria for commercial CAR T products, and physicians treated patients with bridging therapy at their discretion. The median number of lines of prior treatment was three, ranging from two to nine, and the median time from last relapse or disease progression to CAR T was 86 days (range: 33 to 272 days). Most patients, 42 of 49 (86 percent), were in relapse or disease progression status before CAR T, and most had been assessed for function, comorbidity, cognition, mobility, mood, and nutrition before receiving CAR T. (1)
Baseline assessments showed moderate comorbidities in these patients as follows: median Deyo-Charlson Comorbidity Index score (7) of two (range: two to seven); 27 percent of patients had functional limitation, 44 percent had cognitive impairment, 29 percent had a history of falls, 27 percent had lost weight, and 10 percent had depression. (1) Functional limitation was defined by deficits in basic or instrumental activities of daily living, and cognitive impairment was defined as a Montreal Cognitive Assessment score of less than 26. (8)
Among the 49 patients who received CAR T, the six-month median PFS and OS were 48 percent (95 percent CI, 33 to 63) and 71 percent (95 percent CI, 57 to 84), respectively, at a median follow-up of 179 days for survivors (range: 84 to 470). The complete response rate at 100 days was 51 percent. Importantly, we did not observe a statistically significant difference in PFS or OS between the older or younger cohorts by chronological age, functional limitation, cognition, or comorbidity burden. (1)
The safety and toxicity profiles of the older and younger patients were similar, with similar incidences of grades 3 or 4 cytokine release syndrome and immune effector cell-associated neurotoxicity syndrome. (9), (10) As of the last follow-up, only one treatment-related death occurred within 100 days, in a 69-year-old woman who experienced prolonged cytopenia. An additional patient with a history of prior allogeneic hematopoietic cell transplantation died from influenza pneumonia 129 days post-CAR T infusion. (1)
Context: Advancing Care for Older Patients with LBCL
While no major differences were seen between the older and younger groups of patients treated with CAR T, the sample size was small, and patient selection bias may have played a role. However, we found that geriatric assessment domains that are usually prognostic indicators for patients with lymphoma undergoing chemoimmunotherapy or autologous transplantation were not prognostic in the CAR T setting. Our finding of no excess toxicity aligns with previous studies of several real-world cohorts of CAR T patients, including those with poor performance status where chemotherapy had been associated with significant toxicity and mortality. (11), (12), (13)
In the previously reported ZUMA-1 (NCT02348216) and JULIET (NCT02445248) trials, researchers compared the outcomes of CAR T based on chronological age alone. (2), (3) Here, we identified a significant burden of baseline geriatric vulnerabilities, including functional limitation, multiple morbidities, cognitive impairment, weight loss, decreased mobility, and polypharmacy in our geriatric patients.
At MSK, we are dedicated to improving oncologic and nononcologic outcomes after cancer treatments for our patients. We are currently conducting 18 clinical trials for patients with hematologic malignancies, including participating as one of 77 sites conducting a phase III study of CAR T cell immunotherapy versus standard therapy in patients with recurrent or persistent diffuse large B cell lymphoma (ZUMA-7) and a pilot trial of longitudinal geriatric and neurocognitive evaluations for older lymphoma patients receiving CAR T therapy.
This research was supported in part by a National Institutes of Health/National Cancer Institute Cancer Center Support Grant (P30 CA008748) and a Program Project Grant (P01 CA023766). Dr. Lin acknowledges research support from the Elsa U. Pardee Foundation, the New York State Empire Clinical Research Investigator Program, and the Parker Institute for Cancer Immunotherapy at MSK. This work was partially presented at the American Society of Hematology’s annual meeting in December 2019 in Orlando.
Dr. Lin reports no conflicts of interest. Dr. Perales reports receiving honoraria from AbbVie, Bellicum Pharmaceuticals, Bristol Myers Squibb, Incyte, Merck, Novartis, Nektar Therapeutics, and Takeda. He serves on data and safety monitoring boards for Servier and Medigene, and the scientific advisory boards of MolMed and NexImmune. Research support for clinical trials has been received from Incyte, Kite Pharma (Gilead), and Miltenyi Biotec. For disclosures for the other authors, refer to the Haematologica paper.

