Despite the high incidence of brain metastasis after resection of non-small cell lung cancer (NSCLC), the National Comprehensive Cancer Network guidelines do not recommend central nervous system (CNS) surveillance. However, if patients with a high risk of brain metastasis after surgical resection can be identified, surveillance and prophylactic treatment with CNS-directed therapies may improve outcomes.
Memorial Sloan Kettering Cancer Center (MSK) researchers have made several recent discoveries about the clinicopathologic and genomic features predicting higher-risk lung cancer metastatic disease. These insights have revealed new treatment targets and are informing clinical trial risk stratification.
Stage 1 Lung Cancer: Prognostic Features Associated With a Higher Risk Of Recurrence
A team of 18 MSK experts, including thoracic surgeons and pathologists, has found that commonly reported features can be used to identify patients with stage 1 lung adenocarcinoma with a high risk of recurrence after complete resection.
Their retrospective study was the largest series globally to evaluate associations between clinicopathologic features and disease recurrence in this patient population. The paper was published in the February 2025 issue of the Journal of Thoracic and Cardiovascular Surgery. (1)
Led by thoracic surgeon David R. Jones, MD, Chief of the Thoracic Service and Co-Director of the Druckenmiller Center for Lung Cancer Research, the research team assessed results for 1,912 MSK patients who underwent R0 section for stage 1 lung adenocarcinoma from 2010 to 2020. (1)
The five-year cumulative incidence of recurrence was 12%. Among 250 patients who developed recurrence, 141 (56%) had distant and 109 (44%) had locoregional recurrence. (1)
Features independently related to a higher risk of recurrence were as follows: a higher maximum standardized uptake value of the primary tumor (hazard ratio (HR), 1.04); sublobar resection (HR, 2.04); higher lung cancer grade (HR, 5.32 for grade 2 and 7.93 for grade 3); lymphovascular invasion (HR, 1.70); visceral pleural invasion (HR, 1.54); and tumor size (HR, 1.30). Tumors with three to four high-risk features had a higher cumulative incidence of recurrence at five years of 30% versus 4% for tumors with fewer features. (1)
Key learning from this study included that tumor biological features associated with a poorer prognosis are more strongly associated with recurrence than tumor size. Moreover, aggressive features appeared to be additive. Improved risk stratification will help surgeons identify select patients who may benefit from inclusion in clinical trials of adjuvant therapies.
Moreover, the results of this retrospective study formed part of the basis for a recently opened global phase 3 clinical trial (NCT06564844) evaluating the effects of adjuvant immunotherapy and a bispecific antibody-drug-conjugate in patients with stage 1 NSCLC who are ctDNA-positive or have at least one high-risk pathological feature. Patients with EGFR or ALK alterations are excluded from the trial.
The retrospective study was funded by National Institutes of Health/National Cancer Institute grants. Access disclosures for Dr. Jones.
Study Identifies Clinicopathologic and Genomic Features Associated With Brain Metastasis After Lung Cancer Resection
MSK researchers evaluated features associated with brain metastasis in a retrospective study of 2,660 patients who underwent complete resection of stage 1-3A lung adenocarcinoma between 2011 and 2020 at MSK.
This study was the largest to examine risk factors for brain metastasis after surgical resection of NSCLC and the only one to analyze the topic after resection for lung adenocarcinoma specifically. Led by Dr. Jones, the study was published in JTCVS Open in December 2024. (2)
The cumulative incidence of brain metastasis at 10 years was 9.8%, with a median time from surgery to metastasis of 21 months. Better performance status, lack of extracranial metastasis, stereotactic radiosurgery, and targeted therapy were associated with better survival. The median survival after brain metastasis was 18 months. (2)
Clinicopathologic features associated with a higher risk of brain metastasis were a higher maximum standardized uptake value on PET scan of the primary tumor, neoadjuvant therapy, lymphovascular invasion, and stage 3 disease. (2)
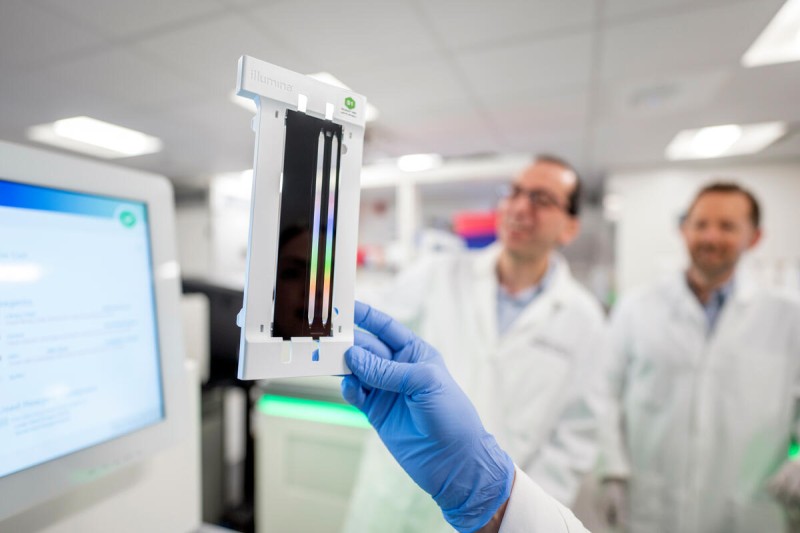
A subset of patients had next-generation sequencing performed on their primary tumor using MSK-IMPACT®. Neoadjuvant therapy, pathologic stage, and TP53 mutations were associated with the development of brain metastasis in this subgroup. (2)
The study was funded by grants from the National Institutes of Health/National Cancer Institute. Access disclosures for Dr. Jones.
TGF-Beta And RAS Signaling Are Both Required For Lung Cancer Metastases
MSK researchers recently discovered activation of both the TGF-beta and RAS signaling pathways is required for the development of lung cancer metastases.
Their study, published in Cell in September 2024, (3) represents years of work led by Joan Massagué, PhD, Chief Scientific Officer and Director of the Sloan Kettering Institute at MSK.
Dr. Massagué is known for his pioneering work, which revealed key insights into transforming growth factor-beta (TGF-beta) signaling processes that promote metastatic growth. For this study, Dr. Massagué and his team recruited collaborators from across the Sloan Kettering Institute and Memorial Hospital who contributed their multidisciplinary expertise.
The research team found that a transcription factor controlled by RAS plays a critical role in metastasis, known as the RAS response element binding protein 1 (RREB1). They discovered that RREB1 cooperates with a signaling complex called SMAD4 that is controlled by TGF-beta. (3)
Further, inhibiting RREB1 disabled metastatic processes in mouse models, suggesting it could be a potential new drug target for addressing metastatic lung cancer. (3) Read more.
Refer to the paper to review the extensive list of funding organizations that provided grants supporting this study, including the National Institutes of Health, various philanthropic foundations and programs, and the Fiona and Stanley Druckenmiller Center for Lung Cancer Research at MSK.
Patient-Derived Organoid Model Informs Immune-Priming Strategy for Individual Patients
Led by Dr. Jones, the MSK researchers created the first in vivo metastasis model to investigate the biology of human lung cancer metastases. The model represents a valuable resource for identifying genes related to brain metastasis. The paper was published in October 2024 in Cell Medicine Reports. (4)
For the model, they used lung adenocarcinoma patient-derived organoids with preserved biologic features of human metastases. Whole genome and RNA sequencing results showed that the model can be used to study clonality and tumor evolution and to identify biomarkers associated with metastasis to specific organ sites. (4)
The model helped the investigators determine the efficacy of treatments to suppress metastasis and identify mechanisms of drug resistance. For example, the model was highly useful in showing how KRASG12C- mutant lung adenocarcinoma responded to the targeted inhibitor sotorasib.(4)
Additionally, when cocultured with autologous peripheral blood mononuclear cells, the model demonstrated that it may help determine the optimal immune-priming strategy for individual patients with lung adenocarcinoma. (4)
The study was supported by grants from the National Cancer Institute, the National Institutes of Health, the Hamilton Family Foundation, and the Department of Defense. Access disclosures for Dr. Jones.
Read more about MSK’s research into new treatment approaches for patients with lung cancer metastatic disease: