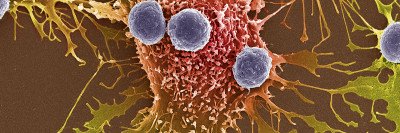
Since 2011, the immunotherapy drugs called checkpoint inhibitors have become an increasingly important treatment for certain cancers. This is especially true for people with melanoma and lung cancer.
Early on, investigators observed that these drugs are extremely effective for some people, even eliminating their cancer entirely. Unfortunately, they don’t work at all for many others. Considerable research has tried to understand why this is the case and exactly how these drugs work.
Memorial Sloan Kettering physician-scientist Timothy Chan has focused on these efforts. He is one of the corresponding authors of a study published November 7, in Nature Medicine that reports a new way to determine who is most likely to benefit from immunotherapy. The findings may help explain why immunotherapy works differently in people around the world.
“Our results help solve part of the mystery of why there is such a large variation in the effectiveness of immune checkpoint drugs,” says Dr. Chan, who leads the Immunogenomics and Precision Oncology Platform at MSK. “It’s important that future clinical trials of immune checkpoint drugs take our discovery into account. This is especially important for international phase III trials.”
Looking to Evolution and Population Diversity for Answers
For decades, the human leukocyte antigen (HLA) genes have been known to govern how the immune system responds to foreign substances in the body. Over thousands of generations, as early humans migrated out of Africa and around the planet, they evolved variations in their HLA genes. These changes protected them from infectious organisms that were found in different parts of the world.
“The classic battle between pathogens and the human immune system plays out in the HLA genes,” Dr. Chan says. A 2017 study from Dr. Chan was the first to show that HLA genes are important for the body’s ability to see cancer after immunotherapy as well. That study reported that people who had a greater number of different copies, or alleles, in their HLA-1 genes responded better to immunotherapy compared with those whose HLA-1 genes had fewer alleles. The new study builds on this previous work.
To quantify how efficient the immune system is at detecting cancer, the researchers looked at the HLA genes from more than 1,500 people who had received immune checkpoint drugs as part of clinical trials at MSK and other hospitals. Most of those included in the study had melanoma or non-small cell lung cancer, but other kinds of cancer were also represented.
People inherit one copy of HLA-1 from each parent. For each person analyzed, the team found that the more molecularly diverse, or different from each other, the two copies of each of their HLA-1 genes were, the more likely someone was to respond to treatment and survive their cancer. The investigators developed a novel way to measure this difference, which they call HLA evolutionary diversity (HED).
Dr. Chan’s co-corresponding author on the Nature Medicine paper, Tobias Lenz of the Max Planck Institute for Evolutionary Biology in Germany, is an expert in the evolution of the human immune system and the HLA genes. Research fellow Diego Chowell and graduate student Chirag Krishna from Dr. Chan’s lab and graduate student Federica Pierini from Dr. Lenz’s lab were the co-first authors.
Recognizing Tumors as Foreign
Dr. Chan has also looked at other factors that make immune checkpoint drugs more effective. In 2014, he led the first studies finding that patients who responded to these drugs tended to have a large number of gene mutations in their tumors. This is known as having a high tumor mutational burden (TMB). When tumors have a greater number of mutations, it is more likely that they will produce proteins that the immune system hasn’t seen before.
“For checkpoint inhibitor drugs to be effective, the immune system needs to be able to recognize cancer cells as foreign,” Dr. Chan says. “High TMB and diverse HLA genes are two sides of the same coin. Both make it more likely that the immune system will see the cancer.”
The researchers note in their study that high TMB and high HED are independent of each other, but the combined outcome of the two led to benefits from immunotherapy drugs that were greater than either of these effects on their own. “These are the yin and yang of T cell–based immune checkpoint treatment,” Dr. Chan says. “High TMB is less useful if a person is unable to present the mutations to the immune system. Having a high HED allows that to happen.”
Finding New Ways to Measure Genetic Diversity
Recent immunotherapy clinical trials have begun to include TMB in their evaluation of how effective checkpoint inhibitors are, Dr. Chan notes. “But among different trials, there is great variation in the role that TMB plays. No one has been able to figure out what’s going on,” he says. “It turns out, we should also be looking at HLA diversity. This finding may account for the unexplained variation that’s seen in the role of TMB in immunotherapy trials.”
He adds that it may also account for the different response rates that have been observed in different parts of the world. HED can vary dramatically depending on where someone lives.
The investigators are now working to develop a standardized way to report HED, so that it can be incorporated into future clinical studies. Dr. Chan’s team is in the process of evaluating HED with industry partners using global phase III trial data. They hope that this measure can eventually become a regular part of cancer diagnosis and be used to match people with cancer with the most personalized treatments.