The Paul Marks Prize for Cancer Research was created by the Boards of Memorial Sloan Kettering Cancer Center to honor the late Paul Marks, who served as President and CEO of MSK for almost 20 years, beginning in 1980. Awarded every other year since 2001, the prize recognizes a new generation of leaders in cancer research who are making significant contributions to the understanding of cancer or are improving the treatment of the disease through basic or clinical research.
The winners of the 2021 prize were announced in November 2021. They will present their work at a series of online lectures hosted by MSK in March 2022.
Here, one of the winners, Ralph DeBerardinis, discusses his career and his current research. Dr. DeBerardinis is a professor at the Children’s Medical Center Research Institute at the University of Texas Southwestern and an investigator in the Howard Hughes Medical Institute.
How did you get interested in cancer research?
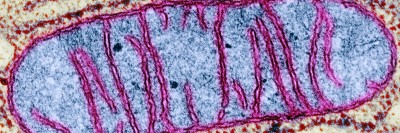
I trained in pediatrics and medical genetics at Children’s Hospital of Philadelphia. As a medical genetics resident, I became interested in diseases called inborn errors of metabolism, which are caused by mutations in genes encoding metabolic enzymes. Many of these diseases can be treated by avoiding fasting and other stresses that cause the body to break down fats and proteins. So I started to think a lot about how those pathways of degradation could be inhibited.
At the end of my clinical training, I started a postdoc with [now-MSK President and CEO] Craig B. Thompson [who was then at the University of Pennsylvania]. I wanted to work in a lab interested in metabolism at the cellular level, particularly studying why rapidly growing cells are so good at producing macromolecules like lipids and proteins. At that time, Craig was one of the only people interested in this question. Cancer biologists of course knew that tumors have high metabolic activity, but almost no one wanted to study why or how.
I’ve had my own lab for about 14 years. These days, about half of my lab studies cancer metabolism and the rest studies links between gene mutations and metabolic disorders, especially in children. In my clinical practice, I treat pediatric patients with inborn errors of metabolism and other genetic diseases.
How do you go about studying the metabolism of cancer cells?
Not that long ago, we thought that tumors had more or less homogeneous metabolic preferences — in other words, we thought they all had similar metabolic needs and used similar pathways to satisfy those needs. But that view has changed. First, we’ve learned that different cancer cells analyzed under identical conditions have very different metabolic features. Because metabolism is controlled by specific cancer-related pathways, it’s possible to use these features to identify genetically defined metabolic dependencies.
Second, until recently, almost all of what we knew about cancer metabolism came from experiments in tumor tissues or cells studied outside of the body. We realized that the same methods used to study metabolism in culture could be applied to real tumors, even tumors growing in patients. So we developed ways to probe tumor metabolism directly in patients. This research tells us which pathways are active in the tumor, how the metabolism differs between the tumor and surrounding tissue, and which activities predict how aggressive the tumor will be.
We’ve learned that metabolism in tumors is quite different from metabolism of cultured cells. So now we are trying to understand why these differences exist, what they can teach us about how metabolism supports cancer progression, and whether inhibiting key pathways prevents progression.
What are you working on today that could impact patient care?
At this point, we’ve studied hundreds of patients with about a dozen different kinds of cancer. That has allowed us to learn how metabolism differs among tumor types and to find pathways that are selectively required for tumor growth in humans and animal models. Ultimately, we hope to define metabolic liabilities that can be targeted with new drugs to treat cancer.
What has become apparent over the past five years is that the metabolic needs of malignant cells evolve as the cancer progresses. This is important, because most patients who die of cancer have tumors that developed drug resistance, spread to new sites, or both. We’re trying to identify the metabolic properties most important for therapy resistance and metastasis, and to see if blocking those activities reduces or prevents disease progression.