Mutations in the KRAS gene are the primary driver of pancreatic cancer. A new class of drugs known as KRAS inhibitors is showing initial promise in clinical trials, but many tumors quickly develop resistance to the treatment.
Now, researchers at Memorial Sloan Kettering Cancer Center (MSK) have discovered a new mechanism of resistance to KRAS inhibitors that suggests an opportunity to make the treatment more effective. Their findings, in mouse models, were published July 8 in Cancer Discovery.
Moreover, the study identified that a more aggressive subtype of pancreatic tumor is likely to respond well to KRAS inhibitors — and potentially even better with a combination therapy.

“Our study suggests treatment could be improved by targeting cancer cell populations that are acutely resistant to KRAS inhibition early, before secondary genetic mutations can arise in response to treatment and increase resistance,” says study first author Anupriya Singhal, MD, PhD, a member of MSK’s Gastrointestinal Oncology Service and postdoctoral researcher in the laboratory of senior study author Tuomas Tammela, MD, PhD.
New treatments for pancreatic cancer are desperately needed. While the overall five-year survival rate for pancreatic cancer is slowly improving, it remains discouragingly low — just 13%, according to the American Cancer Society. And the odds are even worse if the cancer is discovered after it has spread to other organs.
The Two Subtypes of Pancreatic Cancer: Basal and Classical
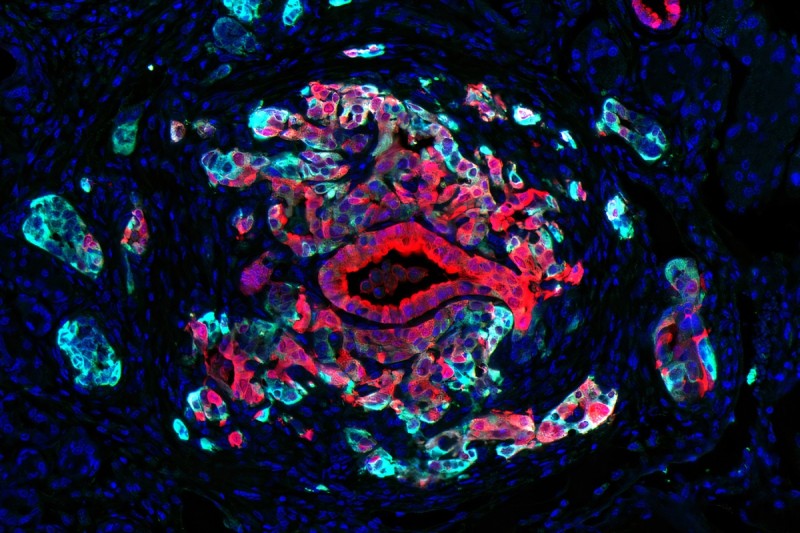
There are two main subtypes of pancreatic cancer, and KRAS is the primary genomic driver of both of them. But the two types have important differences, depending on which other genes are activated in the cancer cells.
- The “basal” subtype of tumor is more aggressive, and patients have a poorer prognosis.
- The “classical” subtype is relatively less aggressive and responds better to chemotherapy.
In reality, however, single-cell RNA sequencing has shown both subtypes contain a mix of both cell types, with one or the other being predominant, Dr. Singhal says.
“One of the most interesting findings in our study is that the more aggressive basal-state cells respond really well to KRAS inhibitors, and these patients who are facing the worse prognoses are the most likely to benefit from the new class of drugs,” she says. “We also found that the classical-state cells within a tumor that don’t respond well to KRAS inhibition are left intact and actually drive the regrowth of the cancer.”
Making KRAS Inhibitors More Effective Against Pancreatic Cancer
The study findings suggest that using KRAS inhibitors at the same time as either chemotherapy or targeted drugs could greatly improve the effectiveness of the treatment and hurt the tumor’s ability to evolve resistance and regrow, says Dr. Tammela, a cancer biologist at MSK’s Sloan Kettering Institute.
“In our animal models, both standard chemotherapy and genetic techniques to target classical cells led to a roughly 70% reduction in tumor size and strongly delayed relapse compared to a KRAS inhibitor alone,” he says. “Our data demonstrate that classical-state cells that survive KRAS inhibitor treatment have the capacity to regrow tumors — and that approaches that eliminate classical cells strongly improve the response to KRAS therapy.”
Along with traditional chemotherapy, which can damage healthy cells as well as cancer cells, there are targeted drugs that have been developed against other types of cancer that may also work well against the molecules found on the surface of classical-state cells in pancreatic cancer, Dr. Singhal adds.
The KRAS inhibitor used in the mouse model studies is an investigational drug made by Mirati Therapeutics called MRTX1133.
MRTX1133 is currently being tested in a phase 1/2 clinical trial for people with advanced pancreatic cancer and other solid tumors that have KRAS G12D mutations. MSK is one of the trial sites.
Additionally, the research team hopes to leverage the study findings to test other approaches in clinical trials at MSK.
Additional Authors, Funding, and Disclosures
The study had 17 additional authors from MSK, Columbia University, Weill Cornell Medicine, and Mirati Therapeutics. A full list of authors can be found in the article.
This work was supported by the National Cancer Institute (R37-CA244911, K12 CA184746, P50 CA257881-01A1, P30-CA08748), Break Through Cancer, Josie Robertson, the American Cancer Society, Rita Allen, the V Foundation, and the American Society of Clinical Oncology.
The study relied upon MSK’s Integrated Genomics Operation Core (funded by Cycle for Survival, and the Marie-Josée and Henry R. Kravis Center for Molecular Oncology), Flow Cytometry Core, Laboratory of Comparative Pathology, and Histology Core.
Dr. Tammela is a scientific advisor with equity interests in Lime Therapeutics; his spouse is an employee of and has equity in Recursion Pharmaceuticals. The Tammela laboratory receives funding from Ono Pharma unrelated to this work.
Read the study: “A classical epithelial state drives acute resistance to KRAS inhibition in pancreas cancer,” Cancer Discovery. DOI: 10.1158/2159-8290.CD-24-0740