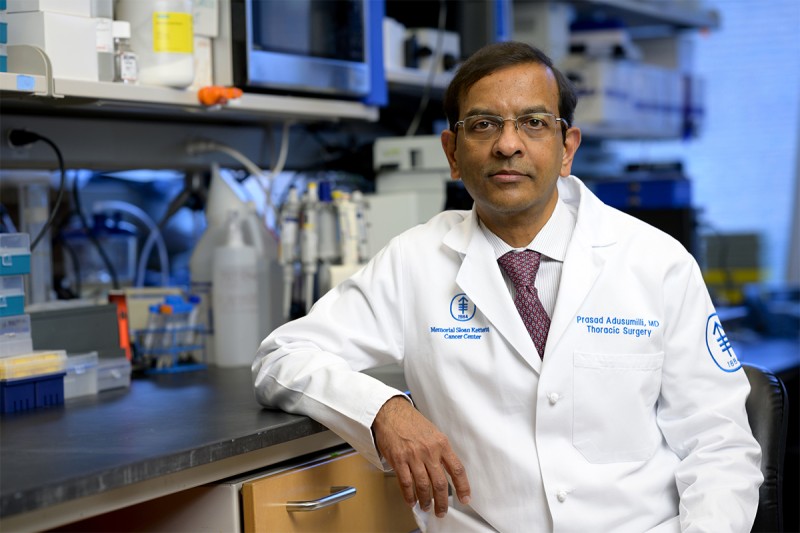
Dr. Prasad Adusumilli says a new way of engineering CAR T cells could improve treatment of solid tumors, which so far have proved resistant to this form of immunotherapy.
Chimeric antigen receptor (CAR) T cell therapy, an immunotherapy that uses genetically modified immune cells, has shown great promise for the treatment of blood cancers such as leukemia and lymphoma. However, this type of immunotherapy has so far been much less effective against solid tumors, which account for most cancers.
A big problem is that solid tumors have a surrounding ecosystem — called the tumor microenvironment — that inhibits attacking CAR T cells.
“The CAR T cells are not powerful enough to overcome this inhibition and kill the cancer cells,” says thoracic surgeon Prasad Adusumilli, MD, a CAR T cell researcher at Memorial Sloan Kettering Cancer Center (MSK). “They go to the tumor site, but then their attack against the cancer peters out.”
Now Dr. Adusumilli’s laboratory has developed a way to boost CAR T cells’ power and persistence by co-opting one of cancer’s own weapons: a genetic mutation in a gene called c-KIT. This mutation is critical to the ability of cancer cells to grow, multiply, and survive.
In lab studies, adding mutated c-KIT to the CAR T cells enabled them to gain strength and fight the tumor longer. The researchers also could regulate the c-KIT effect with a drug, like turning a volume knob up or down. This could allow the therapy’s power to be harnessed more safely.
The researchers report their findings in the June 19 issue of Nature Cancer.
Exploiting a Weapon That Cancer Uses To Gain Strength
Dr. Adusumilli says his team got the idea of using a cancer mutation after noticing how solid tumors reprogram themselves to defend against treatments. Remarkably, the cancer cells can shape their microenvironment and gain strength by mutating a single gene.
“It’s been both fascinating and frustrating to see how cancer cells learn to overcome even new therapies,” Dr. Adusumilli says. “I’ve been thinking of different approaches for making CAR T cells more powerful against solid tumors. And then the light bulb went off — why can’t we exploit a gene mutation that a cancer cell uses to gain strength for our treatment and give cancer a dose of its own medicine?”
Creating a Stronger CAR T Cell
The lab members looked at the various mutations that give cancer cells their power, weighing which would be most suitable to weaponize in the CAR T cells.
“We decided the best approach would be to pick a mutation that has been thoroughly studied and very well understood,” Dr. Adusumilli says. “This is a potentially high-risk approach, so we thought it best to have a mutation for which effective therapies already exist — that way we can block it if something goes wrong.”
In the end, c-KIT was selected. The c-KIT mutations are found in many cancers, and a particular c-KIT mutation called KITv, has been extensively studied. Many Food and Drug Administration-approved targeted therapies called tyrosine kinase inhibitors are effective at blocking this mutation.
In addition, KITv offered an important advantage. Researchers recently learned that fighting solid tumors requires the CAR T cells to use a signaling pathway called interferon gamma. (Interferon gamma is a molecule that plays an important role in immune function.) This signaling pathway has been shown to be critical for CAR T cells to kill solid tumors. The researchers chose KITv in part because it enhanced the interferon gamma signal in the CAR T cells.
Inserting the KITv Mutation Into CAR T Cells
After choosing KITv as the mutation, the researchers needed to insert it into the genome (complete set of genetic material) of the CAR T cells. The genomic region they selected creates proteins involved in an essential part of activating T cells, including CAR T cells. This region has the two signals needed to trigger the T cells. Just as a car you have started doesn’t accelerate without a gas pedal, T cells need an additional signal to rev them up. This second signal is known as a costimulatory signal.
In the past, scientists have incorporated costimulatory signals called CD28 or 41BB into CAR T cells. While these CAR T cells work well against blood cancers, they are not strong enough for solid tumors.
Dr. Adusumilli’s team test-drove the new KITv CAR T cells in animals with human tumors from mesothelioma, lung, and prostate cancers. These new model CAR T cells showed stronger anti-tumor effects than the old model with only CD28 or 41BB. The KITv CAR T cells retained their ability to self-renew and sustain the fight — and without toxicity. What’s more, when added to CAR T cells containing the CD28 signals, KITv was even more efficient and powerful against cancer cells.
Learning From the Enemy Has Many Advantages
All told, Dr. Adusumilli says KITv offers many benefits:
- Its power can be regulated somewhat by a drug.
- It works through the interferon gamma pathway to foil immune-suppressing effects.
- It can be added to CAR T cells along with other costimulatory domains, rather than replacing them, so nothing from current CAR T treatments is sacrificed.
- As a final bonus, the KITv CAR T cells appear to be superior at destroying cancer cells with low levels of the target antigen. CAR T cells often are not strong enough to eliminate cancer cells that have low levels of the antigen that they have been engineered to target and destroy — a problem known as antigen escape.
Dr. Adusumilli’s team is applying for grants to test KITv CAR T cells in a clinical trial (research study) for solid tumors, likely in mesothelioma patients first. He credits MSK’s Office of Technology Development for providing critical funding for the preclinical research that led to this point.
“Translating this approach to the clinic will be challenging, but it also holds great potential,” he says.
And his team appreciates the irony of turning cancer’s weapons against it. A research brief written by Dr. Adusumilli and MSK colleague (and study co-author) Meriem Taleb, PhD, concludes with a quote from the Dalai Lama: “Your enemy is your greatest teacher.”


