A leading scientist whose discoveries about prostate cancer led to lifesaving treatments is now shedding light on an emerging and deadlier form of the disease: neuroendocrine prostate cancer (NEPC).
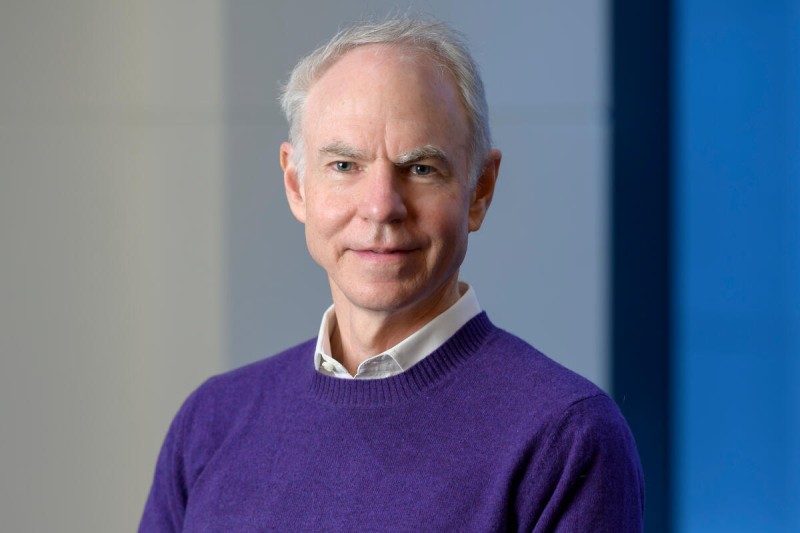
Most prostate cancers are classified as adenocarcinomas, which rely on a protein called the androgen receptor (AR) to survive and grow. Over the past decade, several effective AR-targeting drugs have become available. Memorial Sloan Kettering Cancer Center (MSK) physician-scientist Charles Sawyers, MD, played a critical role in drawing attention to AR as a prime therapeutic target.
These drugs have saved many lives, but some people grow resistant to AR therapies.
In recent years, Dr. Sawyers and MSK colleagues made a surprising discovery about why this happens: Prostate cancer cells can completely change their identity to escape the effects of AR-targeting drugs. This capacity, known as lineage plasticity, allows prostate cancer cells to transform from adenocarcinoma into neuroendocrine prostate cancer, a much more aggressive and deadly form of the disease.
The cellular shapeshifting causes neuroendocrine prostate cancer to develop in 15% of patients receiving androgen receptor therapy. This makes NEPC the second-most common type of this disease. And it’s especially deadly: The median survival rate of someone with neuroendocrine prostate cancer is only 18 months.
Now a team led by Dr. Sawyers has developed a powerful new research tool for understanding how this transition unfolds. The new platform makes it possible to observe the switch in cell states from the earliest stage, enabling researchers to tease apart the genetic mutations and cell-to-cell signals critical to the lineage change. It also is helping to shed light on the role played by the surrounding cells, known as the tumor microenvironment.
“There is an urgent need to understand what drives this transformation in order to develop better treatments,” Dr. Sawyers says. “This new research platform enables us to identify the molecular factors involved in this transition at different stages.”
ASCL1 Protein Helps Drive the Transition to NEPC
Using this new tool, his team has already made one key discovery: The transition from adenocarcinoma to NEPC depends on a protein called ASCL1. Disabling the gene making this protein can prevent the transition.
But the timing is critical.
Deleting the Ascl1 gene before the transition starts can keep adenocarcinoma from turning into NEPC. However, if the cancer has already become NEPC, disabling Ascl1 will merely cause temporary tumor regression. The cancer comes roaring back as several distinct histological variants, including an even more aggressive NEPC.
The results are reported in Nature Cancer.
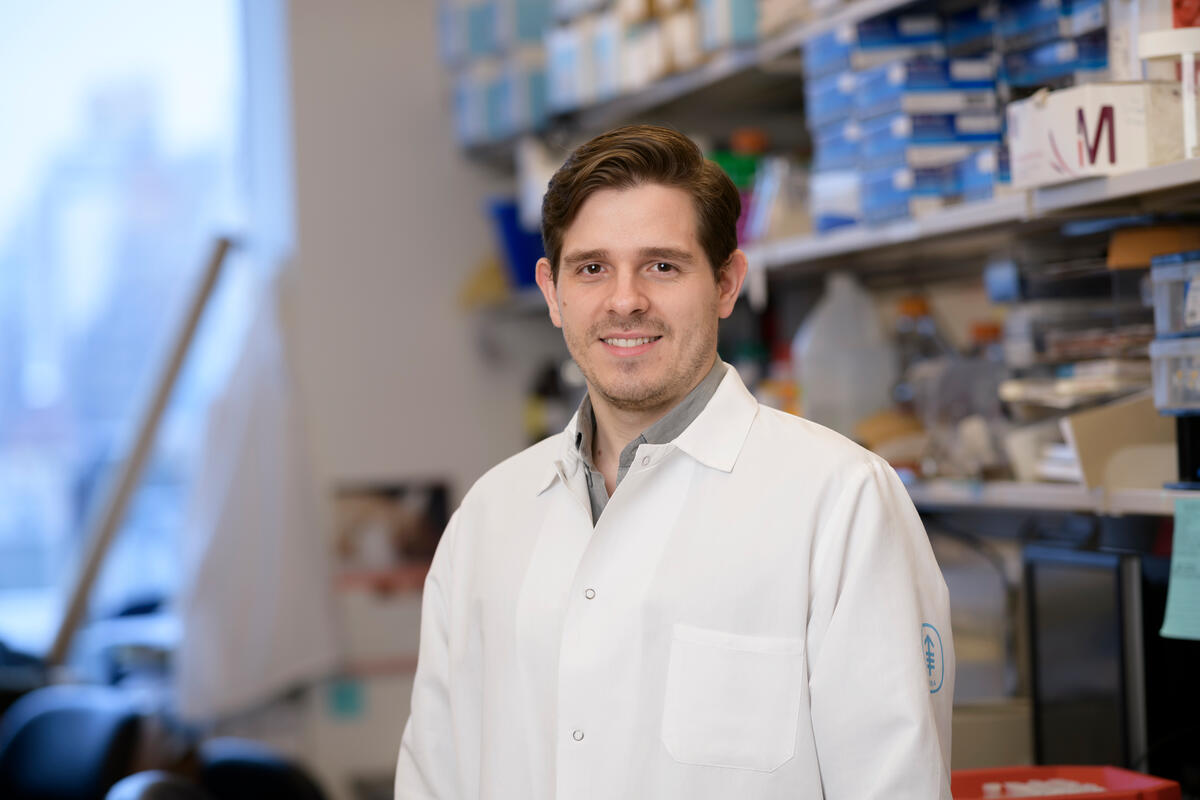
“This research suggests ASCL1 is a good candidate as a drug target,” says Rodrigo Romero, PhD, a research fellow in the Sawyers Lab and the study’s first author. “But it also points to the importance of intervening early in people with prostate cancer that is likely to become NEPC.”
New Research Platform Gets Answers Faster
Previous research from Dr. Sawyer’s lab used a genetically engineered mouse model for prostate cancer. Dr. Romero says that a limitation of these models is that they take time to create.
“If you are interested in a gene like Ascl1, to understand its function you would need to create a strain with the Ascl1 gene deleted and crossbreed it with another strain, and then observe how that deletion affects the biology,” says Dr. Romero. “That can take months or even years.”
The new research platform provides answers much faster. The researchers take normal mouse prostate glands and grow them as organoids — 3D structures composed of cells grouped together and spatially arranged like an organ or tissue. Using a gene-editing technology called CRISPR, researchers can selectively delete specific genes in organoids and then transplant them into mice, which clarifies the role that a given gene plays both in the normal functioning of a cell and in the development of cancer.
“We thought Ascl1 might be key to the transition, but we needed solid evidence,” Dr. Romero says. “With this platform we were able to identify it as essential to the transformation in just three months.”
Research to Develop ASCL1-Focused Treatment for Neuroendocrine Prostate Cancer
Currently no drugs exist that target ASCL1. The protein is a transcription factor, which is involved in the process of transcribing DNA into RNA, the first step in gene expression.
“Transcription factors are notoriously difficult to generate small-molecule drugs against,” Dr. Romero says. “But we’ve seen great progress in targeting proteins once thought to be undruggable — like KRAS — and several groups are working on targeting transcription factors.”
Going forward, the researchers plan to continue disabling other genes, one by one, to get a comprehensive picture of which genes must be turned on or off to cause the transition to NEPC. It’s possible Ascl1 needs to cooperate with other genes — or requires signals from other cells in the tumor microenvironment — before it goes into overdrive.
For example, the researchers suspect a gene called Rb1 must be mutated for ASCL1 to initiate plasticity, and perhaps other signals from the microenvironment are required. Clues for potential cooperating genes may emerge from a computational and systems biology approach pursued in collaboration with the laboratory of computational biologist Dana Pe’er, PhD.
Clarifying the different players will be essential for identifying biomarkers that indicate which patients with adenocarcinoma are most at risk for the prostate cancer transition into NEPC. If researchers can stratify patients into different risk groups, it would help guide clinical decisions.
“If we track patients while they are on treatment, it might eventually make sense to switch the higher-risk patients off AR drugs onto a more neuroendocrine-targeted therapy,” Dr. Romero says. “But we need to develop a much more comprehensive data set to get a clearer picture of what drives the transformation. This research platform allows us to get these answers much faster.”


