Marc Scarduffa was blindsided when he learned he had stage 3 rectal cancer.
Fit and strong as he celebrated his 50th birthday, he had scheduled a colonoscopy simply because he knew he had reached the recommended age to begin screening for colorectal cancer (the recommended age has since been lowered to 45).
Marc had no symptoms, no family history of the disease, and every expectation of a clean bill of health.
However, he woke up after the procedure to grim news. He recalls the doctor telling him, “You have a major tumor, buddy. You need to get to an oncologist.”
So began a journey that would bring Marc to Memorial Sloan Kettering Cancer Center (MSK). At MSK, he found a new approach to rectal cancer that not only successfully treated his disease but did it with less toxic treatments that caused fewer side effects and provided a better quality of life.
It’s part of the intense focus across MSK to help people facing cancer live their best lives during and after treatment.
Rectal Cancer Treatment Without Radiation Therapy
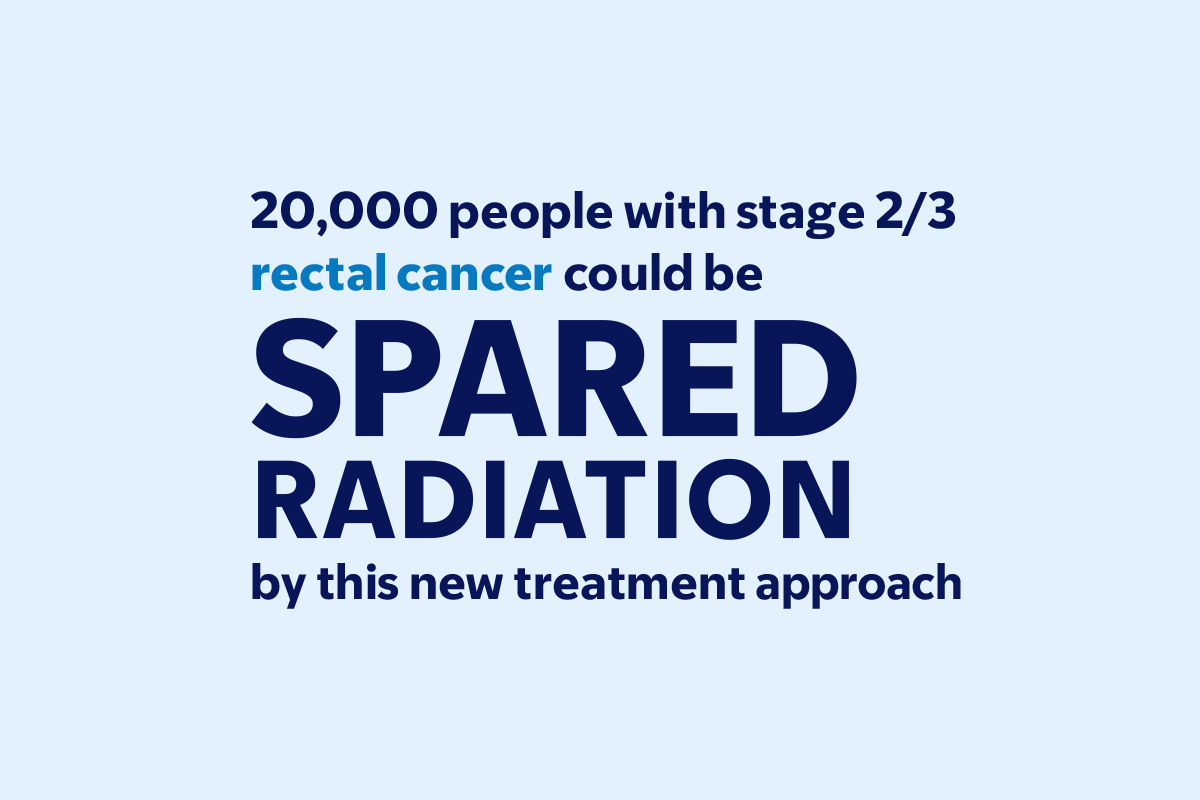
For Marc, the key was a clinical trial investigating whether people with rectal cancer that has not spread (metastasized) could be spared radiation therapy. Since 1990, the standard of care for rectal cancer has been chemotherapy and radiation, followed by surgery.

Led by gastrointestinal oncologist Deb Schrag, MD, MPH, who is also Chair of the Department of Medicine, the successful results of the clinical trial that included Marc were announced in June 2023 at the America Society of Clinical Oncology, the country’s largest cancer conference. The study was also published in The New England Journal of Medicine.
Dr. Schrag started the trial with a hypothesis: Could changing the chemotherapy regimen typically given before surgery allow patients to skip radiation altogether? Preliminary evidence suggested it was possible.
Dr. Schrag hoped eliminating radiation would spare people serious side effects, which can include infertility.
“My colleagues and I began seeing more young women with rectal cancer who were devastated — not just because they had cancer but because the standard treatment we had to offer them would mean that they would not be able to carry a pregnancy to term,” Dr. Schrag says. “That was one of the big reasons we looked for a way to help patients — and to see if we could achieve favorable outcomes without the uniform application of radiation.”
People facing rectal cancer, says Dr. Schrag, are also anxious about other long-term consequences of radiation, which can damage sexual and bowel function.
There are also concerns about radiation and its impact on bone marrow, which makes blood. “Most of your bone marrow is made in the pelvic bones,” explains Dr. Schrag. “When you radiate those bones, the bone marrow resilience can be impaired, which makes it more difficult to give chemotherapy if cancer comes back.”
Marc says he also heard about radiation side effects from other people with cancer. “I was happy to not have to undergo radiation therapy. Among other things, no radiation meant I didn’t have to lose my hair, which I was very enthusiastic about.”
‘MSK Is the Gold Standard’
The trial, led by Dr. Schrag and involving more than 1,100 patients, was a bold move — if it worked, it would upend 20 years of standard practice. The trial divided participants into two separate arms. Before undergoing surgery, half of the patients were given the standard treatment: radiation plus a chemotherapy called 5FU.
The other half received no radiation before surgery. Instead, they were given the chemotherapy regimen called FOLFOX, which for two decades has been given after surgery. But switching the order of treatments by administering FOLFOX first would prove to have major benefits.
For Marc, chemotherapy alone had only minor side effects. “Most people didn’t know I had cancer, and I continued to travel for work,” he says.
The success of his treatment, along with the focus on his quality of life and the compassion of his care team — including gastrointestinal oncologist Leonard Saltz, MD, and colorectal surgeon Martin Weiser, MD — convinced Marc that “MSK is the gold standard for cancer care.”
He adds, “I’m such a big fan of MSK, and I’ve told several people with cancer to go there.”
MSK physicians are also advancing other options for people with colorectal cancer by applying the principles of precision medicine. In a landmark study involving the 8% of patients whose tumors have a specific genetic makeup, MSK researchers successfully treated the cancer with immunotherapy alone, allowing patients to skip the usual treatment of radiation, chemotherapy, and surgery, which can have life-altering side effects.
Similar studies are underway to see if the approach can be used to treat other cancer types.
Treating Prostate Cancer With Ultrasonic Waves

An innovative approach at MSK also helped John Brannan “get a new lease on life” after he was diagnosed with prostate cancer.
A doctor at another hospital suggested surgery as soon as possible. But John was troubled after two people he knew who had undergone similar surgery described persistent side effects, which can commonly include urinary and sexual problems.
John learned of an MSK clinical trial for people like him with intermediate-risk prostate cancer and decided to participate. Led by urologic cancer surgeon Behfar Ehdaie, MD, the trial investigated a treatment known as MRgFUS, which uses high-intensity focused ultrasonic waves guided by magnetic resonance imaging (MRI).
“We believe this novel treatment strategy will improve the lives of many prostate cancer patients,” says Dr. Ehdaie. “Instead of removing all the tissue in the prostate, we have learned that it is safe and effective to treat specific areas and greatly reduce the burden on patients.”
‘No Cuts, No Bruises, No Pain — and Home the Same Day’
The treatment uses focused ultrasonic waves — precisely guided by MRI imagery — to heat the cancer cells inside the prostate to more than 158 degrees (70 degrees Celsius), which kills them.
“Using only sound waves means patients have no cuts, no bruises, no pain — and go home the same day,” says Dr. Ehdaie.
John walked out several hours after his treatment and returned to the hotel where he was staying with his wife and had dinner. “It was pretty much back to normal right away,” he says. “It’s a phenomenal use of technology.”
Dr. Ehdaie now teaches fellow specialists at other centers how to use the novel treatment. He is also preparing for a phase 3 clinical trial scheduled to begin in 2024 that will compare the technology with standard-of-care treatment to test each method’s effectiveness and safety.
MSK specialists are just as determined to help people with prostate cancer who are not candidates for this treatment, including people with more advanced disease.
For instance: “In radiation therapy, we’re constantly trying to design our treatments to minimize side effects,” says radiation oncologist Sean McBride, MD, MPH. Part of that effort, he explains, is listening to patients.
“When a patient has options between different radiation choices, we try to find out what’s most important to them,” he says. “Perhaps its sexual function, bowel function, or urinary function. There are subjective factors that guys bring to the table that help us hone our recommendations.”
Seeing the Whole Patient

A plan that was carefully tailored to personal needs also proved invaluable for Vivian Moore.
At age 80, she was diagnosed with triple-negative breast cancer, a particularly aggressive form of the disease. While some people her age may have wondered whether undergoing treatment with potentially hard side effects would be worth it, she never considered foregoing cancer care.
“I felt comfortable there,” she says, having been cared for by MSK 10 years earlier for bladder cancer. “And I had a lot of confidence that their team would get me through whatever I was facing.”
MSK crafted a treatment plan for Ms. Moore based on her stamina and other needs, with input from breast cancer experts who have special training and experience treating patients over age 65, including Ms. Moore’s MSK breast oncologist, Diana Lake, MD.
“We felt the whole team looked closely at my mom’s individual case to determine what treatments she could tolerate,” says Ms. Moore’s daughter, Nicole. “They didn’t make assumptions based on her age but took a very holistic approach.”
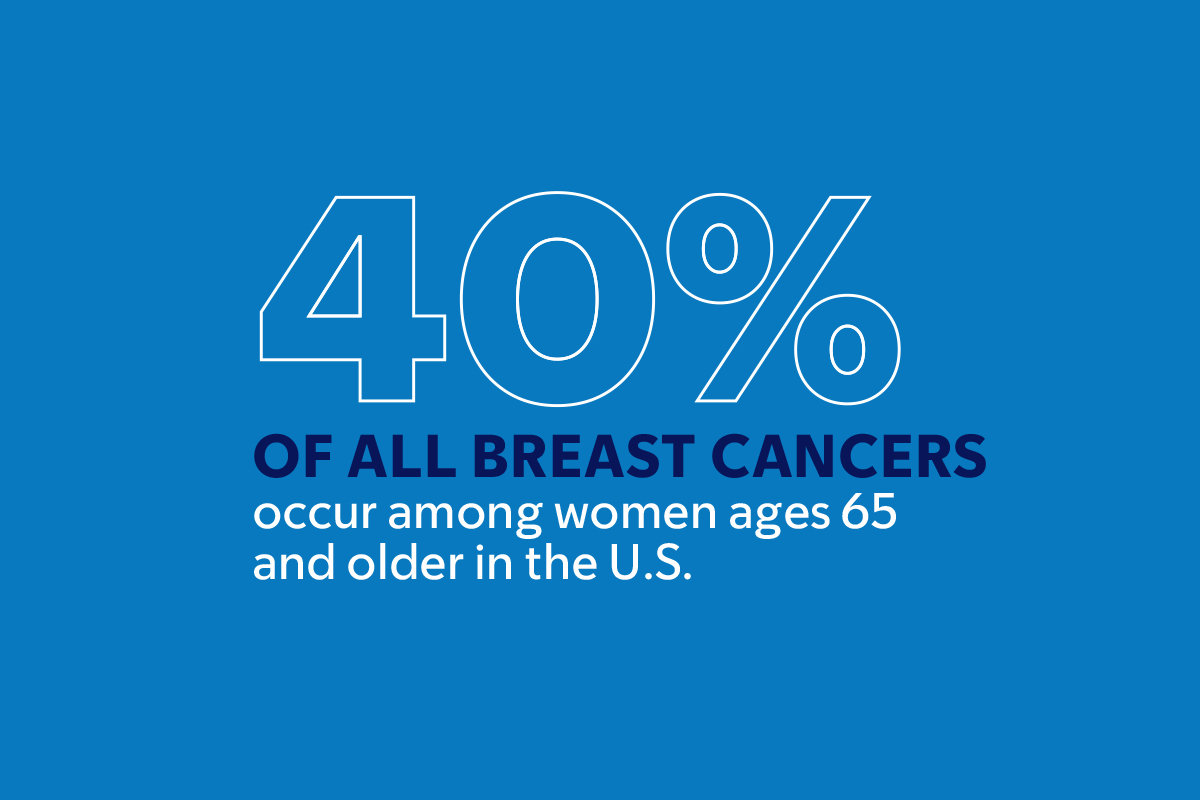
These patients are just the latest example of MSK’s innovation, seeking to use the least amount of treatment to achieve the most benefit. At any stage of life, the cancer experts at MSK are determined to find new ways to reduce side effects and preserve quality of life for the people in their care.
Dr. Schrag’s research receives essential philanthropic support from the MSK Giving community.
Dr. Schrag holds the George J. Bosl Chair.
Dr. Weiser holds the Stuart H.Q. Quan Chair in Colorectal Surgery.