This information describes what urinary tract infections (UTIs) are and why you keep getting them. It describes risk factors, causes, and treatments for UTIs. It explains how you can prevent or stop them.
About your urinary tract
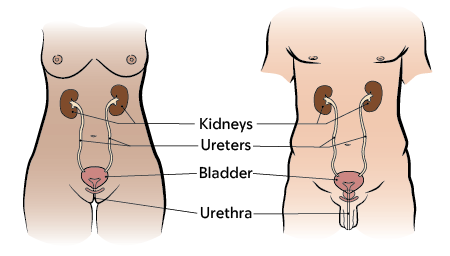
Your urinary tract stores and removes the urine (pee) in your body. The urinary tract is made up of your kidneys, ureter, bladder, and urethra.
What is a UTI?
A UTI happens when the urinary tract, usually the bladder, gets infected. UTIs are more common in people with a vagina, but anyone can get a UTI.
What is a recurrent UTI?
A recurrent UTI is when you keep getting infections. The UTI happens more than 2 times in 6 months, or 3 times in 12 months (1 year).
Signs and symptoms of UTIs
Signs and symptoms of UTIs and recurrent UTIs are the same. They include:
- Dysuria (dis-YOOR-ee-uh): Pain or burning when you urinate (pee).
- Urinary frequency: Having to pee often, usually more than 8 times a day.
- Urinary urgency: Having a strong, sudden need to pee right away.
- Hematuria (HEE-muh-TOOR-ee-uh): Foul-smelling or bloody urine.
- Fever of 100.4 °F (38 °C) or higher.
Some UTIs do not cause symptoms and do not need treatment.
Risk factors for recurrent UTIs
A risk factor is anything that raises your chance of getting a health condition. Risk factors that can cause recurrent UTIs affect both people with a penis and people with a vagina. These include:
- Kidney or bladder stones. These stones can hold harmful bacteria (germs) that cause infection.
- Not emptying your bladder all the way when you urinate, or holding in your urine. Harmful bacteria can grow in your bladder if you hold urine in for too long. Do not hold in urine for more than 3 to 4 hours.
- Urinary catheterization (YOOR-ih-NAYR-ee KA-theh-ter-rih-ZAY-shun). This is a procedure that drains urine from the bladder using a catheter.
- Diverticulum (DY-ver-TIH-kyoo-lum) or pus pockets connected to the urethra. These small pouches can bulge out the urinary tract.
- Nervous system conditions that affect the bladder. This includes neurogenic bladder (when the bladder does not work the way it should). It’s caused by tumors in the brain or spine.
Risk factors for recurrent UTIs for people with a vagina
People with a vagina may have more risk factors for recurrent UTIs. The vagina has helpful bacteria that stop bladder infections. The normal pH level (acidity level) of the vagina is between 3.8 and 8. The risk of UTI goes up if these bacteria are blocked, or if the pH level of the vagina changes.
Here are some more risk factors for recurrent UTIs in people with a vagina:
- Menopause. A lack of estrogen in the vagina makes it easier for harmful bacteria to grow. Estrogen is a hormone that helps keep a healthy vaginal pH and microbiome (MY-kroh-BY-ome). The microbiome is all the microorganisms and viruses that live in a part of the body.
- Sexual intercourse (sex). Bacteria from the vagina can get pushed into the urethra during sex.
- Using spermicide. Spermicide is birth control to stop sperm from getting to an egg. It can kill off the helpful good bacteria in the vagina.
- Douching. Douching is washing or cleaning the inside of the vagina. This is most often done with water or other mixtures of fluids. Douching can lower helpful bacteria in the vagina and change vaginal pH. To lower your risk of getting a UTI, avoid douching if you can.
Poor rectal hygiene. Not wiping well enough after pooping can cause bacteria from the rectum to get into the urethra. This can also happen if you have diarrhea (loose or watery poop) or fecal incontinence. Fecal incontinence is when you cannot hold your poop until you get to a toilet.
How to diagnose a UTI
If you have symptoms, the best way to diagnose a UTI is with a urine culture sample. This will show if you have an infection, and what is causing it. This test will help your care team decide the best treatment plan for you.
If you get treated at an urgent care or primary care, ask for a urine culture. This should not be a rapid test (dip) unless you have a negative dip.
How to treat recurrent UTIs
It’s important to treat anything that changes the way your bladder works. Your healthcare provider can do a physical exam and assess your health history.
In some cases, you may need imaging tests, such as:
- CT scan.
- Renal ultrasound. This test uses sound waves to take pictures of your kidneys, ureter, and bladder.
- Cystoscopy (sis-TOS-koh-pee). During this procedure, your healthcare provider looks inside your bladder using a cystoscope (small, flexible camera).
Your healthcare provider will look at possible risk factors causing your recurrent UTIs.
They will use this information to come up with a treatment plan. This may include surgery or medicine to help you have infections less often. For most people, however, surgery cannot fix what is causing UTIs.
If you have had 2 UTIs within 6 months, even after following a treatment plan, call your MSK healthcare provider. We may be able to prescribe medicine, especially if sex causes a UTI right away.
How to lower your risk of recurrent UTIs
Here are some proven ways to or lower your risk of recurrent UTIs.
Have cranberry juice or supplements
Having cranberry juice or cranberry supplements, such as powder or tablets, help lower the risk of UTIs.
Use vaginal estrogen replacement
This treatment adds estrogen to the vagina and makes it harder for harmful bacteria to grow. It is often used to treat people in perimenopause and post menopause (after menopause). Menopause happens 12 months after a person’s last menstrual period. Perimenopause is the time before menopause and can last for 7 to 14 years. During perimenopause, estrogen levels change and gradually get lower.
You will need a prescription for vaginal estrogen therapy. It is generally safe, but it is not recommended for everyone. Talk with your healthcare provider to see if it is right for you.
Take methenamine
Methenamine (MEH-thuh-nuh-meen) is a prescription medicine that helps fight harmful bacteria in your bladder. You’ll need a prescription from your healthcare provider to get methenamine. Take it with vitamin C. This helps change the pH of your urine and helps the medicine work better.
Other ways to lower the risk of recurrent UTIs
Here are some other possible ways to prevent or lower the risk of recurrent UTIs.
Take probiotics
These can help you keep more of the helpful bacteria that fight off bladder infections. Probiotics are not recommended for everyone. Talk with your healthcare provider to see if taking probiotics is right for you.
Take D-Mannose, GennaMD, or TheraCRAN
These are natural over-the-counter supplements. They keep bacteria from sticking to your urethra and getting into your bladder. Over-the-counter means you do not need a prescription to get them. You can buy these at your local health food store, pharmacy, online at GennaMD, or on Amazon.
Drink enough water each day and urinate every 2 hours
We recommend drinking 8 to 10 cups (about 2 to 2 ½ liters) of water each day. If it’s hard to drink that much, try to drink at least 6 1/2 cups (1.5 L). Your urine should be clear or have a light-yellow tinge. Practice urinating at regular times throughout the day. Do not hold in urine for more than 3 to 4 hours.
Eat a high fiber diet
A high fiber diet has at least 25 grams of fiber a day. Fruits, vegetables, and whole grains are some good sources of fiber. Avoid or limit highly processed foods, added sugars, red meat, and drinks with alcohol. Talk with your healthcare provider or clinical dietitian nutritionist to learn more.
When to call your healthcare provider
If you think you have symptoms of a UTI, call your healthcare provider right away. This includes:
- Feeling burning when you urinate.
- Having urine that smells very bad.
- Having cloudy urine.
- A fever of 100.4 °F (38 °C) or higher.
- Blood in your urine when you pee.
- Trouble emptying your bladder.
- Other symptoms of overactive bladder.
- Body shaking.
- Chills.
- Confusion, if you are 80 years old or older.
