This information explains what a cystocele is and how it’s treated.
What is a cystocele?
A cystocele (sis-tuh-seal) is when your bladder moves and pushes on the outside wall of your vagina (see Figure 1). This happens when the muscles between your bladder and vagina weaken and loosen. A cystocele is also called a prolapsed bladder.
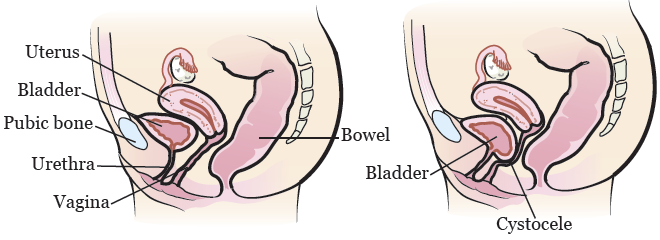
Figure 1. Female anatomy without (left) and with (right) a cystocele
A cystocele can be caused by:
- Aging.
- Vaginal deliveries of heavy babies.
- Menopause (a permanent end of your monthly periods).
- Obesity (having a high, unhealthy amount of body fat).
- Frequent straining during bowel movements (pooping).
- Heavy lifting.
- A hysterectomy (surgery to remove your uterus) or other gynecologic surgery.
Treatment for a cystocele
Treatment for a cystocele includes cystocele repair surgery, surgery to place a urethral sling, or both.
Cystocele repair surgery
A cystocele repair is a surgery to put your bladder back in its normal place. Your surgeon will fix the wall between your bladder and vagina. This will keep your bladder from moving again.
Urethral sling surgery
A urethral sling is a piece of mesh that holds your urethra in its correct position. The urethra is the tube that carries urine (pee) out of your body. Your surgeon will loop the sling around your urethra and attach the ends to your pubic bone (see Figure 2). The sling is permanent.
If you’re having cystocele repair surgery and getting a sling, your surgeon will place the sling during your surgery. Some people get a sling without having cystocele repair surgery. Your healthcare provider will talk with you about what would work best for you.

Figure 2. Female anatomy with urethral sling
Risks of cystocele treatment
Most people who have cystocele repair surgery do not have problems after their surgery. Rarely, the following problems can happen:
- Urine leakage.
- Narrowing of the vagina.
- Painful sex.
- Wearing away of the material on the sling, if you had one placed.
- Injury to your bladder or ureters. Ureters are tubes that take urine from your kidneys to your bladder.
-
Long-term or permanent problems urinating. To help with this, you may:
- Have to insert a catheter (a thin, flexible tube) into your bladder to drain your urine.
- Need another surgery to correct the problem.
- Not being able to hold your urine until you reach a toilet.
- Wearing away of the sling into the vagina, urethra, or bladder. If this happens, your doctor may need to remove the sling.
- The cystocele may come back with time.
The day of your cystocele repair
What to expect when you arrive
Many staff members will ask you to say and spell your name and birth date. This is for your safety. People with the same or similar names may be having a procedure on the same day.
When it’s time to change, you’ll get a hospital gown, robe, surgical head covering, and nonskid socks to wear.
Meet with a nurse
You’ll meet with a nurse before surgery. Tell them the dose of any medicines you took after midnight (12 a.m.) and the time you took them. Make sure to include prescription and over-the-counter medicines, patches, and creams.
Your nurse may place an intravenous (IV) line in one of your veins, usually in your arm or hand. If your nurse does not place the IV, your anesthesiologist (A-nes-THEE-zee-AH-loh-jist) will do it in the operating room.
Meet with an anesthesiologist
You’ll also meet with an anesthesiologist before surgery. They will:
- Review your medical history with you.
- Ask if you’ve had any problems with anesthesia in the past. This includes nausea (feeling like you’re going to throw up) or pain.
- Talk with you about your comfort and safety during your surgery.
- Talk with you about the kind of anesthesia you’ll get.
- Answer questions you have about anesthesia.
During your cystocele repair surgery
During your cystocele repair surgery, your surgeon will make a small incision (surgical cut) in your vaginal wall. If you’re having a sling placed, they will make 2 smaller incisions on your lower abdomen (belly) or inner thigh.
After your cystocele repair surgery
In the Post-Anesthesia Care Unit (PACU)
You’ll be in the PACU when you wake up after your surgery. A nurse will be keeping track of your temperature, pulse, blood pressure, and oxygen levels. You may get oxygen through a tube resting below your nose or a mask over your nose and mouth. You’ll also have compression boots on your lower legs.
Dressing and catheter
You’ll have a gauze dressing in your vagina to help stop bleeding. A catheter will drain urine from your bladder while the area heals. A member of your care team will take these out the day after your surgery before you leave the hospital.
You’ll go home 1 day after your surgery. You’ll have mild vaginal bleeding. Make sure you have sanitary napkins (pads) at home.
Your body will absorb your sutures (stitches) in 7 to 14 days (1 to 2 weeks). You won’t need to have them taken out.
Safety instructions
You can shower 48 hours (2 days) after your surgery. Do not take tub baths, swim, or sit in a pool or hot tub. Ask your healthcare provider when it is safe to do these things.
Do not have sex or put anything in your vagina for 6 weeks after your surgery. This includes tampons.
Do not lift anything heavier than 10 pounds (4.5 kilograms) for 6 weeks after your surgery. Avoid high-energy exercise for 3 months after your surgery. This includes running or jogging, bike riding, and heavy lifting.
Ask your healthcare provider when it is safe to go back to work and doing your everyday activities. This will depend on the type of work you do. Most people can go back to work 2 to 6 weeks after surgery.
Showering
You can shower when you go home after your surgery. Do not bathe or soak in a pool or hot tub until your healthcare provider says it’s safe.
Bladder spasms
While you’re recovering, you may have bladder spasms that can cause urine leakage. While they may feel uncomfortable or even painful, try not to take any medicine for them. It will take longer for you to be able to urinate (pee) normally if you take medicine to prevent the spasms.
Follow-up care
- Make an appointment to see your healthcare provider 2 weeks after your surgery.
- Do not lift anything heavier than 10 pounds (4.5 kilograms) for 6 weeks after your surgery.
- Avoid strenuous exercise, such as running or jogging, for 6 weeks after your surgery.
- Do not have sex or put anything in your vagina (such as tampons) for 6 weeks after your surgery.
Take your medicine
You’ll get 3 types of medicine after your surgery:
- An antibiotic. You must follow the instructions on the bottle until all the pills are gone.
- Medicine to relieve pain after surgery.
- A stool softener to keep your bowel movements (poop) soft. Stop taking it if you have diarrhea (loose or watery bowel movements).
When to call your healthcare provider
Call your healthcare provider if you:
- Have a fever of 101 °F (38.3 °C) or higher.
- Have severe bladder spasms.
- Aren’t able to urinate.
- Have pain that doesn’t go away with your pain medicine.
- Have more vaginal bleeding than when you were in the hospital.