Meet with a nurse
You’ll meet with a nurse before your procedure. Tell them the dose of any medicines you took after midnight (12 a.m.) and the time you took them. Make sure to include prescription and over-the-counter medications, patches, and creams.
Your nurse may place an intravenous (IV) line in one of your veins, usually in your arm or hand. If your nurse does not place the IV, your anesthesiologist will do it in the procedure room.
This information will help you get ready to have your drainage catheter with a Uresil disk placed at MSK. It will explain how to care for it at home.
About your drainage catheter
Your drainage catheter is a thin, flexible tube that drains fluid that has collected in your body. When this fluid is infected, it is called an abscess (AB-ses). An abscess may cause fever, pain, or blood test results that are not normal. If the fluid is not infected, you may or may not have symptoms.
About your drainage catheter placement
An interventional (IN-ter-VEN-shun-al) radiologist will place your drainage catheter. An interventional radiologist is a doctor with special training in using image-guided procedures to diagnose and treat disease. They will explain the procedure to you and give you time to ask questions before you sign a consent form. Signing the consent form means that you agree to the procedure and understand the risks.
During your procedure, your doctor will put the catheter through your skin. They will use fluoroscopy (real time X-rays), a computed tomography (CT) scan, or ultrasound to guide the catheter into place. Then they will secure it to your skin with a silicone disk. They will attach the disk to your skin with an adhesive dressing (bandage).
The procedure usually takes less than 1 hour.
After the procedure, your catheter will be attached to a small bag to collect the drainage. The bag will be below the catheter. This lets fluid drain from the catheter into the bag using gravity. Your doctor will give you an idea of how much drainage to expect.
Your doctor will take out the catheter when the fluid and infection are gone.
Often, drainage catheters are placed urgently if you are sick. In some cases, you will be scheduled to come into the hospital for the procedure. If this is the case, follow the guidelines below.
What to do before your procedure
Ask about your medicines
You may need to stop taking some of your usual medicines before your procedure. Talk with your healthcare provider about which medicines are safe for you to stop taking.
We’ve included some common examples below, but there are others. Make sure your care team knows all the prescription and over-the-counter medicines you take. A prescription medicine is one you can only get with a prescription from a healthcare provider. An over-the-counter medicine is one you can buy without a prescription.
It is very important to take your medicines the right way in the days leading up to your procedure. If you don’t, we may need to reschedule your procedure.
Anticoagulants (blood thinners)
A blood thinner is a medicine that changes the way your blood clots. Blood thinners are often prescribed to help prevent a heart attack, stroke, or other problems caused by blood clots.
If you take a blood thinner, ask the healthcare provider doing your procedure what to do before your procedure. They may tell you to stop taking the medicine a certain number of days before your procedure. This will depend on the type of procedure you’re having and the reason you’re taking a blood thinner.
We’ve listed some examples of common blood thinners below. There are others, so be sure your care team knows all the medicines you take. Do not stop taking your blood thinner without talking with a member of your care team.
|
|
Other medicines and supplements can change how your blood clots. Examples include vitamin E, fish oil, and nonsteroidal anti-inflammatory drugs (NSAIDs). Ibuprofen (Advil®, Motrin®) and naproxen (Aleve®) are examples of NSAIDs, but there are many others.
Read How To Check if a Medicine or Supplement Has Aspirin, Other NSAIDs, Vitamin E, or Fish Oil. It will help you know which medicines and supplements you may need to avoid before your procedure.
Diabetes medicines
If you take insulin or other diabetes medicines, talk with the healthcare provider doing your procedure and the healthcare provider who prescribes it. Ask them what to do before your procedure. You may need to stop taking it or take a different dose (amount) than usual. You may also need to follow different eating and drinking instructions before your procedure. Follow your healthcare provider’s instructions.
Your care team will check your blood sugar levels during your procedure.
Weight loss medicines
If you take medicine for weight loss (such as a GLP-1 medicine), talk with the healthcare provider doing your procedure. Ask them what to do before your procedure. You may need to stop taking it, follow different eating and drinking instructions before your procedure, or both. Follow your healthcare provider’s instructions.
We’ve listed some examples of medicines that cause weight loss below. There are others, so be sure your care team knows all the medicines you take. Some of these are meant to be used to help manage diabetes but are sometimes prescribed just for weight loss.
|
|
Diuretics (water pills)
A diuretic is a medicine that helps control fluid buildup in your body. Diuretics are often prescribed to help treat hypertension (high blood pressure) or edema (swelling). They can also be prescribed to help treat certain heart or kidney problems.
If you take a diuretic, ask the healthcare provider doing your procedure what to do before your procedure. You may need to stop taking it the day of your procedure.
We’ve listed some examples of common diuretics below. There are others, so be sure your care team knows all the medicines you take.
|
|
Weight loss medicines
If you take medicine for weight loss (such as a GLP-1 medicine), talk with the healthcare provider doing your procedure. Ask them what to do before your procedure. You may need to stop taking it, follow different eating and drinking instructions before your procedure, or both. Follow your healthcare provider’s instructions.
We’ve listed some examples of medicines that cause weight loss below. There are others, so be sure your care team knows all the medicines you take. Some of these are meant to be used to help manage diabetes but are sometimes prescribed just for weight loss.
|
|
Take devices off your skin
You may wear certain devices on your skin. Before your scan or procedure, some device makers recommend you take off your:
- Continuous glucose monitor (CGM)
- Insulin pump
Talk with your healthcare provider about scheduling your appointment closer to the date you need to change your device. Make sure you have an extra device with you to put on after your scan or procedure.
You may not be sure how to manage your glucose while your device is off. If so, before your appointment, talk with the healthcare provider who manages your diabetes care.
| If you keep your device on, you may need to sign a form. A member of your care team will talk to you about this before your procedure. |
Arrange for someone to take you home
You must have a responsible care partner take you home after your procedure. A responsible care partner is someone who can help you get home safely. They should be able to contact your care team if they have any concerns. Make sure to plan this before the day of your procedure.
If you don’t have a responsible care partner to take you home, call one of the agencies below. They’ll send someone to go home with you. There’s a charge for this service, and you’ll need to provide transportation. It’s OK to use a taxi or car service, but you still need a responsible care partner with you.
| Agencies in New York | Agencies in New Jersey |
| VNS Health: 888-735-8913 | Caring People: 877-227-4649 |
| Caring People: 877-227-4649 |
Tell us if you’re sick
If you get sick (including having a fever, cold, sore throat, or flu) before your procedure, call your IR doctor. You can reach them Monday through Friday from to
After , during the weekend, and on holidays, call 212-639-2000. Ask for the Interventional Radiology fellow on call.
Note the time of your appointment
A staff member will call you 2 business days before your procedure. If your procedure is scheduled for a Monday, they’ll call you on the Thursday before. They’ll tell you what time to get to the hospital for your procedure. They will also remind you where to go.
If you don’t get a call by noon (12 p.m.) on the business day before your procedure, call 646-677-7001. If you need to cancel your procedure for any reason, call the healthcare provider who scheduled it for you.
What to do the day before your procedure
Instructions for eating
Stop eating at midnight (12 a.m.) the night before your procedure. This includes hard candy and gum.
Your healthcare provider may have given you different instructions for when to stop eating. If so, follow their instructions. Some people need to fast (not eat) for longer before their procedure.
What to do the day of your procedure
Instructions for drinking
Between midnight (12 a.m.) and 2 hours before your arrival time, only drink the liquids on the list below. Do not eat or drink anything else. Stop drinking 2 hours before your arrival time.
- Water.
- Clear apple juice, clear grape juice, or clear cranberry juice.
- Gatorade or Powerade.
-
Black coffee or plain tea. It’s OK to add sugar. Do not add anything else.
- Do not add any amount of any type of milk or creamer. This includes plant-based milks and creamers.
- Do not add honey.
- Do not add flavored syrup.
If you have diabetes, pay attention to the amount of sugar in your drinks. It will be easier to control your blood sugar levels if you include sugar-free, low-sugar, or no added sugar versions of these drinks.
It’s helpful to stay hydrated before procedures, so drink if you are thirsty. Do not drink more than you need. You will get intravenous (IV) fluids during your procedure.
Stop drinking 2 hours before your arrival time. This includes water.
Your healthcare provider may have given you different instructions for when to stop drinking. If so, follow their instructions.
Things to remember
- Take only the medications your doctor told you to take the morning of your procedure. Take them with a few sips of water.
- Don’t use cream or petroleum jelly (Vaseline®). You can use deodorant and light moisturizers. Don’t wear eye makeup.
- Remove any jewelry, including body piercings.
- Leave all valuables, such as credit cards and jewelry, at home.
- If you wear contact lenses, wear your glasses instead, if possible. If you don’t have glasses, please bring a case for your contacts.
What to bring with you
- Medicine for breathing problems, such as inhalers, medicine for chest pain, or both.
- A case for your glasses or contacts.
- Your Health Care Proxy form and other advance directives, if you have completed them.
- Your CPAP or BiPAP machine if you use one. If you cannot bring yours with you, we will give you one to use while you’re in the hospital.
What to expect when you arrive
Many staff members will ask you to say and spell your name and date of birth. This is for your safety. People with the same or similar names may be having procedures on the same day.
You will meet the doctor who will place the catheter. They will explain the procedure and ask you to sign a consent form.
Meet with a nurse
You’ll meet with a nurse before your procedure. Tell them the dose of any medicines you took after midnight (12 a.m.) and the time you took them. Make sure to include prescription and over-the-counter medications, patches, and creams.
Your nurse may place an intravenous (IV) line in one of your veins, usually in your arm or hand. If your nurse does not place the IV, your anesthesiologist will do it in the procedure room.
Meet with an anesthesiologist
You will also meet with an anesthesiologist (A-nes-THEE-zee-AH-loh-jist). An anesthesiologist is a doctor with special training in anesthesia. They will give you anesthesia during your procedure. They will also:
- Review your medical history with you.
- Ask if you’ve had any problems with anesthesia in the past. This includes nausea (feeling like you’re going to throw up) or pain.
- Talk with you about your comfort and safety during your procedure.
- Talk with you about the kind of anesthesia you’ll get.
- Answer questions you have about anesthesia.
Inside the procedure room
A member of your care team will bring you into the procedure room. If you don’t have an intravenous (IV) line, your nurse will put one in. They will give you medicine through your IV to make you feel drowsy. They will also give you an injection (shot) of local anesthesia. This is medicine to numb the area where they will place the catheter into your skin.
Then, your doctor will do the placement procedure and secure the catheter to your skin. They will attach the disk to your skin with an adhesive dressing (bandage).
What to do after your procedure
After your procedure, your care team will bring you to the recovery room. You will need to stay in bed until the medicine has worn off. You will then return to your hospital room or go home with your caregiver.
About your catheter
You will have a black mark on the catheter above the disk (see Figure 1). Your nurse will show it to you. This mark should always be the same distance from the top of the disk. If it changes, this means that the catheter has moved. Call Interventional Radiology right away so someone there can check it.

The end of the catheter outside of your body will be attached to a 3-way stopcock (see Figure 2). The stopcock has a tap that you can turn to control the flow. It also has 3 points of attachment.
The drainage bag connects to the attachment point opposite to the catheter. It can be attached to your clothes with a safety pin or secured to your leg with Velcro® straps. The bottom of the bag has a blue twist cap, which you will use to drain the bag.
The third attachment point has a protective cover on it. The cover is called a needleless connector (also called a clave). You can inject fluids through here.
CathGrip® is a device that helps keep your catheter in your body in case you accidentally pull on it. Always use CathGrip while your catheter is in place.

Showering
You can take showers, but you need to keep your dressing dry. If the dressing gets wet, you will need to change it. Wet dressings are a common cause of skin problems.
Before you shower, take off the belt and empty the drainage bag. Tape the drainage bag to your body near the catheter or use a strap to attach it to your waist.
Cover your dressing to keep it dry. Tape plastic wrap or a gallon-sized bag over the dressing to keep it dry. You can also use AquaGuard®, which is a one-time use waterproof cover to protect your dressing. A hand-held shower can help direct the water away from the dressing.
Putting on the AquaGuard
Follow these instructions to put on the AquaGuard. You’ll still need to use a Uresil dressing. Do not use AquaGuard to replace the Uresil dressing.

- The edges of the AquaGuard have peelable tape. Fold over a corner of each side of the tape (see Figure 3). Do not let the tape on the AquaGuard touch the dressing. It can lift the dressing when you take off the AquaGuard after showering.
- Hold the AquaGuard with the arrows pointing towards your head. Peel off the top strip and place the top edge of the AquaGuard above the dressing. Smooth it down.
- Grab a folded corner and peel down one side, smoothing it as you go.
- Do the bottom and remaining side the same way.
- When you’re done showering, take off the AquaGuard and throw it in the trash.
How to care for your drainage catheter
Your nurse will teach you how to care for the catheter. Use this resource at home to remind you of what you learned. A visiting nurse may come help you at home until you or your caregiver feel confident caring for the catheter. Ask your healthcare provider for more information about how to arrange for a visiting nurse.
Every day:
- Check the catheter.
- Flush the catheter with normal saline.
- Record the amount of drainage in the bag.
- Empty drainage from the bag.
Change your dressing and drainage bag once a week. You will also need to change the dressing if it gets loose, wet, or dirty. If a wet dressing is left against your skin, it may make your skin irritated and sore.
You can check the catheter and flush it with the normal saline yourself or ask someone to help you. You may need someone to help you change the dressing and drainage equipment.
Check the catheter
Check your catheter every day. You can use a hand-held or full-length mirror to do this.
- Find the black mark to make sure it is in the correct position near the disk.
- Check the dressing to make sure it is secure. Change the dressing if it is wet, dirty, has come loose, or started to pull away from the skin.
- Check the skin around the catheter when you are changing the dressing. There should be no redness, areas of broken skin, or rash. Fluid should not leak around the catheter.
- Look at the fluid in the bag. It should be flowing freely into the bag. There should be no change in the way it looks.
- Check the catheter and the drainage bag for kinks (bends) in the tubing.
If you see a problem, finish your catheter care, then call your Interventional Radiologists’ office.
Flush the catheter
Flush your catheter with normal saline. Your doctor will tell you how often to do this. Follow their instructions. They will also tell you whether to use 3 milliliters (mL), 5 mL, or 10 mL of normal saline.
Below is a video that shows how to flush a biliary catheter. Follow the same directions to flush your drainage catheter with a Uresil disk.
How To Flush Your Biliary or Abscess Drainage Catheter
-
Gather your supplies. You will need:
- 1 (10 mL) prefilled normal saline syringe
- 2 alcohol wipes
- Wash your hands with warm water and soap for at least 20 seconds or use an alcohol-based hand sanitizer.
- Take the syringe out of the wrapper. Take the cap off the syringe using a twisting motion. Do not let the tip of the syringe touch anything.
With the cap off, remove the air from the syringe. To do this, hold the syringe open side up. Then push the plunger slowly until the normal saline is at the top.
If your doctor told you to flush with less than 10 mL, squirt the extra saline out. Then connect the syringe to the needleless connector on the stopcock and lay it on the table. Do not let the tip of the syringe touch anything.
- Sit or lie comfortably. Turn the stopcock toward the drainage bag (see Figure 2).
- Clean the needleless connector on the stopcock by rubbing it with an alcohol wipe for 15 to 30 seconds.
- Place the syringe onto the needleless connector. Hold the connector while you push and turn the syringe clockwise (to the right) to lock it into position.
- Push the plunger of the syringe to push one-third of the normal saline into the catheter, then pause. Push in another one-third of the normal saline and pause again. Then push the rest of the normal saline into the catheter. Never pull back on the plunger. Always push forward.
Stop and call your doctor’s office if you have any of the following while flushing:
- Feel pain.
- Feel resistance.
- See leaking around the catheter.
Do not try to put in any more saline.
- When the syringe is empty, turn it counterclockwise (to the left) to take it off. Throw it away in your regular trash. Then turn the stopcock back to the direction of the needleless connector. You will probably see fluid drain into the bag.
Emptying the collected drainage from the bag
Measure and empty the drainage twice a day, or more often if needed.
-
Gather your supplies. You will need:
- The measuring container you got in the hospital.
- Non-sterile gloves.
- 2 alcohol wipes.
- Wash your hands with warm water and soap for at least 20 seconds or use an alcohol-based hand sanitizer.
- Put on the non-sterile gloves.
- Clean the cap at the bottom of the drainage bag with an alcohol wipe.
- Twist the cap open while holding it over the measuring container.
- Let the fluid drain into the container. Do not let the bottom of the bag touch the sides of the drainage container.
- When all fluid has drained out of the bag, twist the cap closed.
- Clean the cap with an alcohol wipe.
- Measure the amount of fluid in the container, then flush the fluid down the toilet.
- Wash the measuring container with soap and water. Let it air dry.
- Throw out the gloves. Clean your hands with soap and water for at least 20 seconds, or with an alcohol-based hand sanitizer.
- Record the amount of drainage on the form at the end of this resource. Be sure to subtract the amount of your saline flush (3 mL, 5 mL, or 10 mL) from the daily totals.
Change the Uresil dressing
The Uresil disk is attached to your drainage catheter. The Uresil dressing system covers the disk. This keeps the catheter in place and away from the skin where your doctor placed it.
Change the dressing, stopcock, and drainage system once a week.
Change the dressing if it:
- Gets wet.
- Gets dirty.
- Gets loose.
- Pulls away from your skin.
- Leaks.
You can try to put the equipment together yourself or ask someone to help you. You’ll need someone to help you change the dressing and equipment.
This video shows how to change your Uresil dressing:
-
Gather your supplies:
- 1 Uresil adhesive dressing
- 3M™ No Sting Barrier Film
- Adhesive remover wipe
- Alcohol wipes
- Gauze
- Mild soap and a cup of water
- Non-sterile gloves
- 1 (2 inch x 2 inch) Telfa
- Scissors
- CathGrip kit
- Waste basket
- Wash your hands with warm water and soap for at least 20 seconds or use an alcohol-based hand sanitizer.
-
Clean your scissors with an alcohol pad. If your Telfa is larger than 2 inches by 2 inches, you will need to cut it to that size. Cut a slit in that piece (see Figure 4) and set it to the side.

Figure 4. Cutting slit in Telfa - Sit or lie comfortably. At this point, you will need someone to help you. The person doing the dressing change should follow the instructions below.
- Wash your hands and put on nonsterile gloves.
- Put the drainage bag in a place where it will not fall.
- Hold the silicone disk in place using 1 finger to prevent tension or pulling on the catheter. Find the slit in the Uresil dressing. From this spot, slowly and gently peel the adhesive away from the skin while holding the disk. If the skin around the catheter is sensitive, rub the adhesive remover around the edge of the dressing. This can help ease any discomfort.
- Release the catheter from the straps on the CathGrip. Make sure the drainage bag is somewhere that it can’t fall. If you’re changing the CathGrip, use adhesive remover to release it from the skin.
- Throw out the old Uresil dressing, and the adhesive remover if you used it.
- Wet a gauze pad with soap and water. Use it to clean the skin around and under the Uresil disk. Using the same gauze, clean the top and bottom sides of the disk itself. Always hold one side of the disk firmly on the skin while cleaning under the other side.
- Rinse the skin with a new clean gauze, then dry it with fresh gauze.
- Wipe the top side of the disk with an alcohol wipe. This takes off any soap residue.
- Look at the disk nipple. The black ink mark should be just above the disk nipple (see Figure 1). If it moved, finish changing the dressing and call the doctor’s office.
-
Check the insertion site under the silicone disk. Always hold one side of the disk firmly on the skin while tilting up the other side. Finish changing the dressing and call the doctor’s office if you see:
- Redness.
- Swelling.
- Foul-smelling drainage.
- Leakage of fluid around the catheter.
You may notice new tissue growing around the insertion site. This is harmless, but your doctor can take it off if it is painful.
- Put the 3M™ No Sting Barrier Film on the skin around and under the silicone disk. Then put more on the top of the disk where the dressing will be placed. This protects the skin.
-
Slide the Telfa under the disk, around the catheter (see Figure 5). The slit should point towards the person’s feet. The Telfa will prevent moisture from building up under the disk.
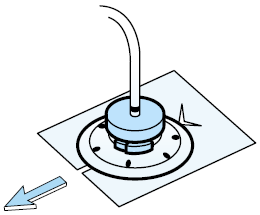
Figure 5. Sliding the Telfa under the disk, around the catheter -
Pick up the Uresil dressing. Open the slit and place it around the catheter (see Figure 6). Line the slit up with the slit in the Telfa. Make sure the dressing is adhesive side down, shiny side up.
Place the dressing over the flat part of the disk, but under the disk’s nipple. The slit in the dressing should point towards the person’s feet. This lets the skin breathe and helps keep the skin from breaking down.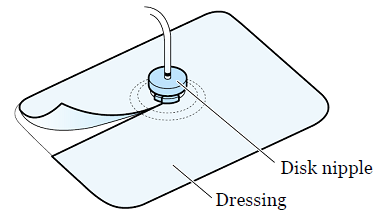
Figure 6. Uresil dressing - The Uresil dressing has 3 pieces of backing. Start at the corner of the biggest piece and slowly peel the backing away. As you peel away the paper, press the adhesive to the skin. This will get easier with practice. If the dressing does not stick properly, take off the Uresil dressing and Telfa and restart at step 15.
- Take off the other 2 pieces of backing paper 1 at a time. Press the adhesive to the skin. Overlap the slit edges of the dressing to make the dressing more secure.
-
If you’re changing the leg drainage bag or the CathGrip, follow the instructions in the sections below. If you are only changing the dressing right now, reattach the catheter to the CathGrip.To attach to the CathGrip, place your catheter on the device straps. There are 2 straps, one with jagged edges and one with holes. The strap with the holes has 2 openings.Put the strap with the jagged edges end into the lower opening of the other strap. Then, pull it to secure it (see Figure 7).

Figure 7. Placing the catheter and removing the paper back of the CathGrip - Take off the gloves and throw them in the wastebasket..
- Write the date of the dressing change on the Uresil dressing so you know when to change it again.
- Wash your hands with warm water and soap for at least 20 seconds or use an alcohol-based hand sanitizer.
Change the stopcock and drainage equipment
Below is a video that shows how to change the equipment on a Uresil disk catheter. Follow the same directions to change the equipment.
-
Gather your equipment:
- Nonsterile gloves
- 1 needleless connector
- 1 sterile 3-way stopcock
- 1 drainage bag
- 1 Cathgrip kit
- Safety pin or strap
- Gauze
- 1-inch Micropore® paper tape
- Waste basket
- Wash your hands with warm water and soap for at least 20 seconds or use an alcohol-based hand sanitizer.
- Open the packages with the needleless connector, 3-way stopcock, and drainage bag. Put the package with the drainage bag to one side.
- Take off the protective cover from the base of the needleless connector and throw it away. Attach the needleless connector to center port of the stopcock (see Figure 2). Then put the stopcock down.
- Take the drainage bag out of the package. Connect the tubing from the drainage bag to the stopcock with a twisting motion. Close the drainage port on the bottom of the bag by turning it clockwise. Closing the port stops it from leaking.
- Place the assembled drainage bag back in its package. This will keep it clean until you are ready to connect it to the catheter.
- Wash your hands again for at least 20 seconds, then put on the non-sterile gloves.
- If you have not done so, release the catheter from the straps on the CathGrip. Make sure the drainage bag is somewhere that it can’t fall.
- If the bag is attached with a safety pin, remove the safety pin. Make sure you can reach the new drainage bag.
- Hold gauze under the connector and twist off the old stopcock and drainage system from the catheter. Throw it away, then quickly attach the new stopcock and drainage system.
- Make sure the off tap of the stopcock is turned in the direction of the needleless connector.
Change your CathGrip
The CathGrip will prevent pulling, tension, or kinking of the drainage catheter and tubing. You will need your CathGrip kit for this part.
- Choose a position for the CathGrip. The CathGrip and drainage bag tubing should be lower than the catheter insertion site. This will let it drain. Make sure it’s lower, both when you are standing and laying down.There should be no pull or tension on the catheter when it is attached. There should be a gentle bowing of the catheter.
- Rest the tubing on the side of your abdomen where you chose to put the CathGrip.
- Check the site where you’ll place the CathGrip. Choose an area that’s not red or irritated. Trim any long hairs at the site with scissors or hair trimmer. Avoid using a razor.
- Open the CathGrip package.
- Clean the site with the alcohol wipe from the kit. This will get rid of oils and products from your skin, such as lotion or soap. Let the alcohol dry completely.
- Wipe the site with the BioPlus+ Skin Prep included in the kit.
- Let the area dry to the touch. This takes about 15 seconds.
- Take off the paper on the back of the CathGrip one side at a time (see Figure 7). Put it on the skin in the desired location. Repeat with the other side.
- Gently press the CathGrip to the skin for 5 seconds to seal it to the skin.
-
Place the catheter on the device straps. There are 2 straps, one with holes and one with jagged edges. The strap with the holes has 2 openings. Insert the strap with the jagged edges end into the lower opening of the other strap. Pull it to secure it (see Figure 8).

Figure 8. Securing the catheter in the CathGrip - Make sure that there is no pull or tension on the catheter. If you notice any tension or pull, change the position of the catheter in the CathGrip.
-
Secure the drainage bag with the strap or with a safety pin. Attach the bag to the waistband of your clothing with the safety pin, or to your leg with the attached Velcro straps. The bag should be below the level of the catheter. This lets the catheter drain using gravity (see Figure 9).

Figure 9. Drainage bag below the catheter - Check to see that the fluid is draining into the new tubing.
- When you have finished, take off the gloves and wash your hands.
Activities while you have your drainage catheter
- You can go to work and exercise with your catheter in place. Avoid movements that involve stretching from side to side or repeated bending. These could cause the catheter to move.
- Do not swim, take a bath, or put your catheter underwater. Talk to your Interventional Radiology doctor if you have a vacation planned. They will teach you what to do in this situation.
- Always keep the tubing secured to your body with a CathGrip.
- When you are getting dressed, be sure not to tug on the catheter. Do not let the tubing become kinked by clothing, such as pantyhose or a belt. Try not to lie on your catheter when you sleep to prevent kinking of the catheter. Clothing can usually cover the catheter and should be loose-fitting (not tight).
When to call your healthcare provider
Call your healthcare provider if you notice any of the following:
- There is no drainage from your catheter when the 3-way stopcock is in the upright position.
- The amount of drainage is much less than usual.
- The drainage looks bloody.
- There is leakage around the insertion site.
- You can’t flush the catheter, or it leaks when it is flushed.
- The location of the black mark has changed.
- There is no longer drainage from the catheter
- The clamp has broken or opened.
- There is a kink in the tube that you can’t straighten out, causing a blockage.
- You have pain, tenderness, or swelling at the catheter site.
- Your skin around the catheter looks red, irritated, or different from the way it normally looks.
- You have a fever of 100.4 °F (38 °C).
- You have any concerns about your catheter.
Ordering supplies
Your healthcare provider will give you enough supplies to last for 2 weeks. You can order more supplies through your visiting nurse service, or your doctor’s office can help you get them. The items and their supply numbers are listed below.
| Item | Supply Number |
|---|---|
| Adhesive Remover (1 box) | 3170 |
| Alcohol Wipes (1 box) | 3330 |
| CathGrip (each) | 2675 |
| Micropore paper tape (1 box) | 3174 |
| Non-sterile gloves (1 box) | 4545 |
| Plain gauze (1 package) | 3424 |
| Skin Prep (1 box) | 3332 |
| Uresil adhesive dressing (1 box) | 3226 |
| Telfa (1 each) | 3327 |
| Drainage bag (1 each) | 3361 |
Prefilled syringes
You will need a prescription for prefilled normal saline syringes. You can get the prescription from the IR clinic.
If your local pharmacy does not have the syringes, you can get them from MSK’s outpatient pharmacy. The pharmacy is located at Memorial Hospital at 1275 York Avenue, between East 67th and East 68th Streets. It is open Monday through Friday from 9 a.m. to 5:45 p.m. To reach the pharmacy, call 646-888-0730.