This information explains your nutritional care during your treatment for esophageal cancer at MSK. It also explains the diet (eating and drinking) changes you can expect during and after your treatment.
It’s important to get enough nutrition before, during, and after your cancer treatment. Getting enough nutrition can help you:
- Stay strong.
- Keep your weight stable.
- Fight infection.
- Have fewer side effects.
- Heal after surgery.
- Prevent nutrition deficiencies such as not getting enough vitamins from the foods you eat.
Read through this resource at least once before your treatment. You may also want to use it as a reference during and after your treatment.
It’s important to follow a well-balanced diet so you get enough nutrition during your treatment. This will help keep your weight stable and maintain your muscles and strength.
About your nutrition during treatment
The usual treatment for esophageal cancer is an esophagectomy (surgery to remove all or part of your esophagus). Some people also have chemotherapy and radiation therapy before surgery. Having chemotherapy and radiation therapy before surgery is called induction therapy. Your doctor will talk with you about which treatment plan may be best for you.
Working with a clinical dietitian nutritionist
Clinical dietitian nutritionists are available to help you plan your diet during and after treatment. They can help make sure you get enough nutrition. To make an appointment with a clinical dietitian nutritionist, call 212-639-7312 or ask a member of your care team to help you.
If you’re having chemotherapy and radiation therapy before your surgery, your clinical dietitian nutritionist can:
- Help you manage your symptoms by changing your diet.
- Help you get enough nutrition.
- Keep you from losing or gaining too much weight.
When your surgery is scheduled, your clinical dietitian nutritionist will call you. They will talk with you about your diet and nutrition before and after surgery. Ask them about any questions and concerns you have.
After your surgery, an inpatient clinical dietitian nutritionist will manage your diet and nutrition. They will teach you about eating and drinking while you’re in the hospital. After you leave the hospital, an outpatient clinical dietitian nutritionist will help you with your diet at home. They will work with you to make sure you get
enough nutrition.
Contact information for MSK Nutrition Services
To make an appointment with a clinical dietitian nutritionist, call 212-639-7312 or ask a member of your healthcare team to help you. MSK offers nutrition services in Manhattan and at many of our regional network locations.
Visit www.mskcc.org/nutrition to learn more about MSK’s nutrition services.
Nutrition during your chemotherapy and radiation therapy
Use the information in this section to make sure you get enough nutrition while you’re having chemotherapy and radiation therapy before surgery. If you have questions about your diet or nutrition, talk with your clinical dietitian nutritionist.
If you’re having a lot of trouble swallowing, you may need to use a feeding tube to help you get enough nutrition. If you do, your healthcare provider will give you more information.
Tips for eating more calories and protein
If you’re eating less than usual during your chemotherapy and radiation therapy, follow a high-calorie, high-protein diet. A high-calorie, high-protein diet can help you stay at the same weight (if you’re at a healthy weight) or lose weight more slowly (if you’re overweight).
High-calorie, high-protein foods
Eat foods from the table below to add more calories and protein to your diet. Ask your clinical dietitian nutritionist for more menu ideas, if you need them.
Choose foods that are easy for you to eat. If you’re having problems that affect how you eat, read the “Tips for managing treatment side effects” section.
| Food group | Food | Calories | Protein (grams) |
|---|---|---|---|
| Meat, beans, and eggs | 1 cup cooked dried beans | 240 | 4 |
| ½ cup chicken salad | 200 | 14 | |
| 1 large egg cooked with 1 tablespoon butter | 175 | 7 | |
| 3 ounces tuna canned in oil | 170 | 25 | |
| ¼ cup egg substitute | 25 | 5 | |
| Nut butters | 1 tablespoon of full fat peanut butter | 95 | 4 |
| 1 tablespoon of almond butter | 100 | 3 | |
| Dairy | ½ cup canned evaporated milk (can be used instead of water when cooking) | 160 | 8 |
| 2% Greek yogurt | 140 | 20 | |
| 5% Greek yogurt | 190 | 18 | |
| ½ cup premium ice cream | 220 | 14 | |
| ½ cup full fat creamed cottage cheese | 115 | 7 | |
| ¼ cup (1 ounce) shredded cheese | 100 | 7 | |
| ¼ cup half-and-half | 80 | 2 | |
| ½ cup whole milk (can be used instead of water when cooking) | 75 | 7 | |
| 1 tablespoon cream cheese | 50 | 1 | |
| 2 tablespoons sour cream | 50 | 1 | |
| Fats | 1 tablespoon butter, margarine, oil, or mayonnaise | 100 | 0 |
| 2 tablespoons gravy | 40 | 1 | |
| Sweets | 1 tablespoon honey | 60 | 0 |
| 1 tablespoon sugar, jam, jelly, or chocolate syrup | 50 | 0 | |
| Meal replacements | 1 meal replacement bar | 200 | 15 |
| 1 scoop (1 ounce) protein powder | 100 | 15 |
High-calorie, high-protein liquid nutritional supplements
Your healthcare provider may suggest taking high-calorie or high-protein nutritional supplements. If they do, take the supplements between meals. If you take them with a meal, they can be filling and may keep you from eating more of your food.
You can buy most of the products in the table below at any supermarket or pharmacy. If you don’t see a product in the store, ask a pharmacist or store manager to order it for you. You can also order these products online.
| Nutritional supplement | Calories | Protein (grams) | Water (mL) | Lactose free? |
|---|---|---|---|---|
| Ensure® Original (8 ounces) | 250 | 9 | 196 | Yes |
| Ensure® Clear (8 ounces) | 240 | 8 | - | Yes |
| Ensure Plus® (8 ounces) | 350 | 13 | 180 | Yes |
| Orgain® Nutritional Shake (11 ounces) | 250 | 16 | - | No |
| Glucerna® Shake (8 ounces) | 220 | 10 | 200 | Yes |
| Boost® Original (8 ounces) | 240 | 10 | 200 | Yes |
| Boost Glucose Control® (8 ounces) | 190 | 16 | 200 | Yes |
| Boost® Nutritional Pudding (5 ounces) | 240 | 7 | 140 | Yes |
| Boost® VHC (Very High Calorie) (8 ounces) | 530 | 22.5 | 168 | Yes |
| Boost Breeze® (8 ounces) | 250 | 9 | 196 | Yes |
| Carnation Breakfast Essentials® Powder | 130 | 5 | - | No |
| Carnation Breakfast Essentials Ready-to-Drink (11 ounces) | 250 | 14 | 285 | No |
| Premier Protein Shakes (Premier Protein) | 160 | 30 | - | No |
| ENU® Complete Nutrition Shake (11 ounces) | 450 | 23 | - | Yes |
| Kate Farms® Komplete® (10.8 ounces) | 290 | 16 | - | Yes |
| Benecalorie® (1.5 ounces) | 330 | 7 | - | Yes |
| Beneprotein® Instant Protein Powder (7 grams) | 25 | 6 | - | Yes |
High-calorie, high-protein nutritional shakes
You can also make your own high-calorie, high-protein nutritional shakes. For shake recipes and other tips for increasing your calorie and protein intake, read Eating Well During Your Cancer Treatment.
Tips for eating more food
Chemotherapy and radiation therapy can cause side effects that may make it hard to eat such as taste changes and appetite loss. If you’re not eating enough food or are losing weight from treatment, follow the guidelines below.
-
Have small, frequent meals.
- Have a half-sized meal every 2 to 3 hours.
- Aim for 6 to 8 small meals a day instead of 3 large meals.
- Create and follow a meal schedule. Don’t wait until you’re hungry.
- Keep your favorite foods in your home where you can get to them easily.
- Buy single-serving food items that you can eat easily. Try small bags of mixed nuts or trail mix.
-
Cook in batches so you have leftovers.
- Keep 1 extra serving in your refrigerator for the next day, but not longer.
- Freeze the other extra servings. When you’re ready to use a serving, thaw it in the refrigerator or microwave, not on the kitchen counter. Then, reheat it until it’s steaming hot.
- Include many different food groups and food types in your diet, unless your healthcare provider tells you not to.
- Get more calories from liquids than solid foods. For example, have milkshakes or nutritional supplements such as Ensure or Carnation Breakfast Essentials.
- Keep your dining experience pleasurable and non-stressful.
- Think of your nutrition as being just as important as your medicine.
Tips for managing treatment side effects
Chemotherapy and radiation therapy can also cause side effects such as:
- Dry or sore mouth or throat.
- Difficult or painful chewing or swallowing.
- Nausea (feeling like you’re going to throw up).
These things can make it harder for you to eat. If you have any of these side effects, follow the guidelines in the next sections.
If you have new side effects or your side effects are getting worse, talk with your healthcare provider about how to manage them.
Problems with chewing or swallowing
Examples of problems with chewing or swallowing include painful or difficult chewing or swallowing or a feeling like food is getting stuck in your throat. If you have any of these side effects:
-
Follow a puréed or mechanical soft diet.
- Puréed foods are foods that don’t need to be chewed. They’re usually blenderized (put into a blender or food processor) to a smooth texture.
- Mechanical soft foods are foods that need less chewing than most other foods. They’re usually diced or chopped.
- Keep a blender (such as a Vitamix®) or food processor in your home. This is helpful if you need to puree your foods.
- Have 1 or more high-calorie drinks every day. These can be ready-to-drink nutrition supplements (such as Ensure or Boost) or homemade milkshakes and smoothies. Talk with your clinical dietitian nutritionist about what may be best for you.
Dry mouth
It can be hard to eat if your mouth is dry and doesn’t make enough saliva. If your mouth is dry:
- Choose soft, moist foods, such as stews and creamed soups, and tender cooked chicken and fish.
- Add gravies, sauces, applesauce, or other liquids to your foods.
- Have a spoonful of warm soup or other liquid between mouthfuls of food.
- Try foods prepared with gelatin, such as mousses. They tend to slide down your throat more easily.
- Always carry a bottle of water with you. You can also try carrying a small, clean spray bottle filled with water. Spray water in your mouth throughout the day to keep it moist.
- Try eating sugar-free mints or lemon drops or chewing sugar-free gum to make more saliva.
- Try an over-the-counter (not prescription) saliva supplement, such as Biotene® Oralbalance Moisturizing Gel
-
If you’re having trouble keeping your weight the same, choose drinks that have calories instead of water. Examples are fruit juices, fruit nectars, and liquid nutritional supplements, such as Ensure.
- If you have diabetes, talk with your doctor or clinical dietitian nutritionist before doing this. They may tell you to limit or avoid sugary drinks to help control your blood sugar.
Mouth sores
If you have mouth sores:
- Moisten dry foods with sauces, soups, fats, and dips.
- Avoid steaming hot foods and drinks.
- Don’t eat acidic fruits (such as oranges, grapefruits, lemons, or limes) or drink acidic fruit juice.
- Don’t eat spicy foods.
- Don’t put vinegar (including salad dressings with vinegar) on your foods if it bothers you.
- Suck on sugar-free candies.
- Gently brush your teeth with a soft-bristle toothbrush before and after meals.
- Rinse your mouth with saline solution (mild salt water). You can make the solution by mixing ¼ to ½ teaspoon of salt into an 8-ounce glass of warm water.
If the things above don’t control your mouth pain, tell your doctor or healthcare provider. They may prescribe a liquid numbing medication to help.
Nausea
Most healthcare providers will prescribe medication to treat nausea or keep it from happening. You can also follow the guidelines below to help manage nausea.
- Try eating low-fat, starchy foods. These foods may be less likely to make you feel nauseous. For example, try rice, white toast, crackers, cheerios, melba toast, angel food cake, pretzels, or saltine crackers.
- Don’t eat spicy foods.
- Don’t eat high-fat foods, especially fried foods, such as donuts, french fries, pizza, and pastries.
- If the smell of food bothers you, try eating your food at room temperature or cold. Avoid foods that are too hot. They often have a stronger smell that can make nausea worse.
- Eat small, frequent meals.
- Chew your food well to make it easier to digest.
- Don’t drink large amounts of liquids at once. This will keep you from getting too full, which can make nausea worse.
- Try sipping on ginger tea, ginger ale, non-alcoholic ginger beer, or sucking on candies containing real ginger. Ginger may be soothing and help with nausea.
Diet and nutrition after your esophagectomy
During your esophagectomy, your doctor will remove part of your esophagus. They will also move your stomach up and connect your stomach to the remaining part of your esophagus (see Figures 1 and 2). They will place a feeding tube in the part of your small intestine called the jejunum (see Figure 2). The feeding tube is called a jejunostomy tube or J-tube. You will use it to get nutrition while your esophagus and stomach heal after surgery.

Figure 1. Your esophagus and stomach before
your surgery.
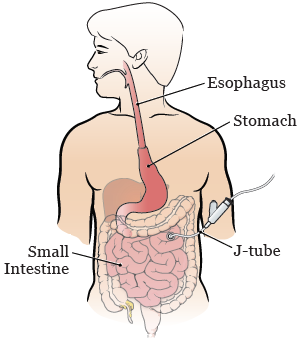
Figure 2. Your esophagus, stomach, and J-tube
after your surgery.
After your esophagectomy, your care team will keep track of your recovery. They will tell you when you can start drinking and eating again. This may be while you’re in the hospital or when you’re discharged from the hospital. Your doctor and inpatient clinical dietitian nutritionist will tell you what to expect.
While you’re in the hospital, an inpatient clinical dietitian nutritionist will manage your nutritional care. They will:
- Check to make sure you’re getting enough nutrition.
- Teach you about your diet and tube feeding schedule.
- Tell your case manager which diet and nutrition supplies you’ll need at home. Your case manager will order these supplies for you.
- Be available to talk with you and answer your questions.
After you’re discharged from the hospital, an outpatient clinical dietitian nutritionist will start managing your nutritional care. They will:
- Call you within 3 days of your discharge.
- Talk with you regularly to help you manage your diet at home.
- Be available to talk with you and answer your questions.
About your feeding tube
Right after your surgery, you won’t be able to eat or drink anything. You will get all of your nutrition from liquid formula put into your small intestine through your feeding tube. The formula can be digested and absorbed by your small intestine. It has all the nutrients your body needs.
Tube feeding rates
Your tube feeding rate is the amount of formula you get through your feeding tube per hour. It’s measured in milliliters (mL) per hour.
Your goal feeding schedule is the tube feeding rate and number of hours that gives you the right amount of calories, protein, and fluids. Your inpatient clinical dietitian nutritionist will calculate your goal feeding schedule based on your height and weight.
At first, you will have a low tube feeding rate. Your tube feeding rate will slowly be increased to your goal rate or schedule.
Tube feedings after discharge
You may get some nutrition from tube feedings after you’re discharged from the hospital. This may be because you’re following a liquid diet, can’t get enough nutrients just from eating, or haven’t yet started drinking or eating. This will be referred to as supplemental. Your tube feedings make sure you get all the protein and calories you need to have a successful recovery.
If you will have tube feedings after discharge, your inpatient clinical dietitian nutritionist will tell your case manager which formula and supplies you will need at home. You and your case manager will work with a home care company to arrange for your tube feeding formula and supplies to be delivered to your home. Make sure you know who your home care company is.
Before you leave the hospital, a person from the home care company will visit your hospital room. They will teach you and your caregiver how to use your tube feeding pump. Your nurse and inpatient clinical dietitian nutritionist will also give you the resource How to Use a Pump With Your Feeding Tube and be available to answer your questions. Make sure you and your caregiver feel comfortable using your tube feeding pump before you’re discharged.
After you’re discharged, you will probably use the same formula that you did in the hospital. You will be on a 16-hour tube feeding schedule. As you heal, you will use the feeding tube for fewer hours. Your outpatient clinical dietitian nutritionist will tell you how many hours you should use your feeding tube. Having a few hours without tube feedings each day will help increase your appetite so you can wean off of the tube feedings more quickly.
Eating and drinking after surgery
As your esophagus and stomach heal, you will slowly start drinking and eating. You will follow different diets as you’re able to drink and eat more things. You will most likely go through these diets in this order.
- Clear liquid diet: This diet includes only liquids that you can see through. Clear liquids are easiest for your body to digest.
- Full liquid diet: This diet includes all the liquids in a clear liquid diet, as well as liquids that are thicker or not clear.
- Soft diet: This diet includes all the liquids in a full liquid diet, as well as foods that are physically soft. This means less chewing is needed to get the food into a texture that’s smooth and easy to swallow.
At first, you will also get nutrition from your feeding tube while you’re following these diets. As you’re able to get more of your nutrition from drinking and eating, your healthcare provider will lower your tube feeding volume. Eventually, your tube feedings will be stopped.
There are more guidelines for each of these diets in the “Resources” section near the end of this resource. If you follow any of these diets while you’re in the hospital, you will get a menu explaining which foods these diets include.
Your clinical dietitian nutritionist will decide when you’re ready to start each new diet. They will also tell you which diet to follow when you go home. Most people follow a clear liquid while still having some tube feedings when they’re discharged.
Clear liquid diet
You will start a clear liquid diet around 6 days after your surgery. To learn more about what you can drink while following this diet, read the “Clear liquid diet” section near the end of this resource.
When you first start following a clear liquid diet, your tube feeding schedule will be shortened from about 24 hours per day to about 18 hours per day. When you’re discharged home, your tube feeding schedule will be shortened to about 16 hours a day, depending on your progress. This will help increase your appetite during the day.
Drink small amounts at a time and drink slowly as you learn your limits. This will help you keep from having reflux. Start with 4 ounces (½ cup) at a time. Aim to drink 4 ounces of liquids 6 to 8 times a day (24 to 32 ounces total) when you first start a clear liquid diet.
Full liquid diet
If you’re able to follow a clear liquid diet, you will start following a full liquid diet around 10 days after your surgery. To learn more about what you can drink while following this diet, read the “Full liquid diet” section near the end of this resource.
When you start following a full liquid diet, your outpatient clinical dietitian nutritionist will give you instructions for how to adjust your tube feeding schedule. Most people keep the same tube feeding rate but lower the number of hours they get tube feeds to 12 hours per day.
You may not be able to drink some or all dairy products after your surgery. Pay attention to the way you feel after having dairy (such as milk and yogurt), and avoid the things that cause discomfort. To learn more, read the “Food intolerances after surgery” section of this resource.
Soft diet
Your outpatient clinical dietitian nutritionist will tell you when you should start following a soft diet. Usually, this is around 13 days after your surgery. For information about what you can drink and eat while following this diet, read the “Soft diet” section near the end of this resource. You can also follow the 6-meal soft diet sample menus included in that section.
When you start following a soft diet, your outpatient clinical dietitian nutritionist will give you instructions for how to adjust your tube feeding schedule. Most people keep the same tube feeding rate but lower the number of hours they get tube feeds to 8 hours per day.
When you start following a soft diet, you should also start tracking your weight and keeping a food and drink log. For more information, read the “Tracking your food and liquid intake” section of this resource.
You may not be able to eat some foods that you could eat before surgery, such as sweets and dairy. Pay attention to the way you feel after eating different foods and keep notes in your log. To learn more, read the “Food intolerances after surgery” section of this resource.
Stopping your tube feedings
Your outpatient clinical dietitian nutritionist will follow up with you often to see how many calories you’re eating and drinking. They will help you slowly reduce the amount of tube feeding formula you get as you get more nutrients from eating and drinking. The goal is for you to stop having any tube feedings and be able to follow a soft diet in small, frequent meals.
Your doctor will remove your feeding tube once you’re able to get enough nutrition from your diet. The goal is to remove your feeding tube during your first follow-up appointment after surgery. This is usually about 2 weeks after you’re discharged from the hospital.
Diet and nutrition timeline
These are goals for your recovery. Your experience may not follow this timeline exactly. Follow your healthcare provider’s instructions for changing your diet.
| Days after Surgery | Diet and nutrition goal |
|---|---|
| 2 |
|
| 5 |
|
| 6 |
|
| 7 |
|
| 10 |
|
| 13 |
|
| 16 |
|
Tracking your weight
It’s important to track your weight after surgery. Weigh yourself about every 3 to 5 days, or as often as your outpatient clinical dietitian nutritionist asks you to. It’s best to weigh yourself around the same time each day. Make sure you’re wearing the same amount of clothes each time.
It’s normal to lose weight right after you’re discharged from the hospital. When you’re first recovering from your surgery in the hospital, your body may hold onto more fluids than usual. This can make your weight go up. After you’re discharged, you will lose this fluid weight. Your weight should return to your normal or slightly below your normal weight. These changes are normal. Your outpatient clinical dietitian nutritionist will work with you to help keep you from losing too much weight.
In the months following surgery, tell your care team if you’re losing weight without trying. Remember that you can make an appointment with an outpatient clinical dietitian nutritionist if you need help with your diet.
Tracking your food and liquid intake
After your esophagectomy, you may feel full quickly or have other digestive changes that affect your eating. Keeping a food and drink log will help you see what foods and portion sizes are easiest for you to eat. It will also help you make sure you’re getting enough calories.
In your food and drink log:
-
Keep track of all of the foods you eat and liquids you drink. Write down:
- The time you eat or drink
- The amount (portion) and type of food or drink
- The number of calories in the food or drink
-
Write down any symptoms or problems you have after eating or drinking.
- Are you feeling too full?
- Do you have pressure in your chest?
- Are you having reflux?
- Are you having pain in your abdomen (belly) or diarrhea (loose or watery bowel movements)?
It’s also important to track your weight. Weigh yourself about every 3 to 5 days, or as often as your clinical dietitian nutritionist asks you to weigh yourself. Weigh yourself around the same time each day. Make sure you’re wearing the same amount of clothes when you weigh yourself.
See the example of a food and drink log below. There is a blank log for you to use in the “Resources” section.
| Time | Portion size | Description | Calories | Symptoms? |
|---|---|---|---|---|
| 7:00 | 4 oz | Apple juice | 60 | None |
| 8:00 | 1 jumbo 5 oz | Scrambled egg Mashed potatoes | 100 160 | None |
| 10:00 | 6 oz | Yogurt | 105 | None |
| 2:00 | 5 oz 4 oz | Mashed potatoes Vanilla pudding | 160 110 | None |
| 4:00 | 1 jumbo | Scrambled egg | 100 | None |
| 6:00 | 6 oz 5 oz ¼ cup ¼ cup | Mashed potatoes Soft cooked butternut squash Stewed chicken Gravy | 92 75 58 50 | Very full, unable to finish meal |
| Daily total 1130 |
Measuring foods
To accurately measure foods, use measuring spoons, measuring cups, or a food scale. You can also use the guidelines below to estimate amounts of some foods (see Figure 4).

Figure 4. Guidelines for estimating portion sizes
Finding calorie information
You can find the calorie information for packaged foods on the nutrition facts label (see Figure 5).

Figure 5. Where to find calorie information on a nutrition facts label
If a food doesn’t have a nutrition facts label, you can look up the calorie information on a nutrition resource website, such as CalorieKing.com or myfitnesspal.com. You can also download the MyFitnessPal application to your smartphone.
Your clinical dietitian nutritionist can calculate the calorie information for you during your scheduled follow-up appointments. Make sure you write down what you eat and drink and how much you have so they can calculate the calories.
Diet guidelines after your surgery
After your surgery, your stomach won’t be able to hold as much as it did before surgery. You will need to have 6 or more small meals a day instead of 3 main meals. This will help you eat the right amount of food, even though your stomach is smaller. Tell your doctor and clinical dietitian nutritionist if you’re losing weight without meaning to.
Guidelines for eating
- When you first start eating, you may only be able to comfortably eat a ½ to 1 cup portion of food at a time. Over time, you will be able to have larger portion sizes. Make sure to eat nutrient dense high calorie and high protein foods.
- Chew your food well. This helps with digestion.
- Eat slowly. This way, you will stop eating before you get too full and feel uncomfortable.
- Don’t drink more than 4 ounces (½ cup) of liquid during your meals. This will allow you to eat enough solid food without getting too full. It will also slow down the digestion of your food. Remember that soup counts as a liquid.
Guidelines for drinking
- Drink most of your liquids at least 1 hour before or 1 hour after your meals. This helps you avoid feeling too full and prevents dehydration.
- Aim to drink about 8 to 10 (8-ounce) glasses of liquid each day. Avoid carbonated (fizzy) drinks if they make you feel full.
Food intolerances after surgery
A food intolerance means you’re not able to have certain types of foods or drinks. After your surgery, you may have some food intolerances that you didn’t have before surgery.
Sugar Intolerance
Some people have cramping, stomach pain, or diarrhea within about 20 minutes of eating foods or drinks that are high in sugar. This is called dumping syndrome. If you have these symptoms, talk with your clinical dietitian nutritionist. They may recommend adding sources of fiber to your diet. Use food labels to keep track of how much sugar you’re eating.
Some people feel weak, hungry, nauseated, anxious, shaky, or sweaty 1 to 2 hours after eating a sugary meal. This is caused by low blood sugar.
Dumping syndrome and low blood sugar can be controlled by changing your diet and watching what you eat. Ask your clinical dietitian nutritionist for more information.
Foods and drinks high in sugar include:
- Sodas
- Fruit juices
- Candy
- Ice cream
- Cakes
- Honey
- Syrups
- Jams
Fat intolerance
Some people have trouble digesting large amounts of fat. Try having small amounts at first, and then increase the amount of fat in your diet slowly.
Foods high in fat include:
- Butter, margarine, and oils
- Mayonnaise
- Creamy salad dressing
- Cream cheese
- Gravies
- Potato chips and corn chips
- Rich desserts
- Fried foods
If your bowel movements (poop) smell worse than usual or are pale, greasy, or floaty, you may not be digesting fats well. If you have any of these symptoms, talk with your doctor or outpatient clinical dietitian nutritionist. You may need a medication to help you digest fats. This is rare.
Lactose (dairy) intolerance
Lactose is a type of sugar found in dairy or milk products. Some people have trouble digesting lactose after having an esophagectomy. This is called lactose intolerance. Symptoms of lactose intolerance include gas, bloating, and diarrhea. These symptoms can happen 30 minutes to 2 hours after having dairy products.
After surgery, slowly bring dairy products back into your diet. Milk, ice cream, and soft cheeses have high amounts of lactose. Hard cheeses, yogurt, and butter have smaller amounts of lactose.
To test your tolerance to dairy foods, start by drinking a 4-ounce (½ cup) serving of milk.
- If you don’t have any of the symptoms of lactose intolerance, you can start eating more dairy foods.
- If you have any of the symptoms of lactose intolerance, you may still be able to eat foods with smaller amounts of lactose. Pay attention to how you feel after having different dairy products.
If you think you may be lactose intolerant:
- Try using a product to help you digest dairy products (such as Lactaid® tablets or drops).
- Try dairy products that are processed to remove the lactose from them (such as Lactaid milk, cottage cheese, and ice cream).
- Ask your clinical dietitian nutritionist for help, if needed.
Sometimes, lactose intolerance that develops after surgery goes away with time. You may want to try dairy products again in a couple of months to see if your stomach can handle them.
Tips for managing common problems
The following are common problems after an esophagectomy. Keeping a food record and writing down any symptoms or problems you have may help you realize why the problems are happening. You can use the blank daily food and drink log in the “Resources” section.
If the tips below don’t help, speak to your clinical dietitian nutritionist or doctor for advice.
Tips for managing reflux
Reflux is when foods or liquids that you swallow come back up your throat into your mouth. This happens because the valve between your esophagus and stomach was removed during your surgery. Follow these tips for managing reflux:
- Sit up straight during meals and for at least 60 to 90 minutes after you’re finished.
- Wear loose-fitting clothes around your abdomen.
- Eat your last meal of the day at least 2 hours before your bedtime.
- Drink your last drink of the day at least 1 hour before bedtime.
- Always keep the head of your bed at a 30-degree angle or higher. Use a wedge pillow to keep your upper body and head raised up. You can buy a wedge pillow at a surgical supply store or online.
- When you bend down, try bending at your knees instead of your waist.
- Don’t eat or drink too much at one time.
Tips for managing nausea
- Avoid foods that are too rich, spicy, or greasy.
- Don’t eat or drink too fast. Try putting your fork down between bites.
- Don’t have too much to eat or drink at one time.
- Don’t lie too flat after meals. Remember that you should be at a 30-degree angle or higher whenever you lie down.
Tips for managing fullness
Your stomach will not be able to hold as much as it did before surgery, and it will be higher in your chest. It may also empty more quickly or slowly for the first few months after surgery. These things mean that you will get full more quickly. Since your stomach is now in your chest, the feeling of fullness might be different. Follow these tips for managing fullness:
- Pay attention to signs of fullness or pressure behind your breastbone. This will help you keep from eating too much and having reflux.
- Don’t have too much to eat or drink at one time.
- Don’t drink too much during your meals.
- Don’t eat or drink too fast. Try putting your fork down between bites. It takes 20 minutes for your brain to realize that you’re full.
- If you’re having trouble having 6 smaller meals instead of 3 large meals, make a meal schedule with set times for meals.
- If you’re finding yourself going back to the larger portions you had before your surgery, try preparing mini-meals ahead of time so they’re readily available.
Tips for managing diarrhea
- Try eating less sugar, then less dairy, then less fat. Pay attention to see if the diarrhea gets better when you cut back on any of these things. If it does, eat less of those foods.
- Try eating foods with soluble fiber, such as canned fruits, bananas, and oatmeal.
-
Make sure you’re keeping foods safe at home.
- Put leftovers in the refrigerator or freezer right away.
- Throw away refrigerated leftovers after 2 days.
- Throw away frozen leftovers after 6 months.
- Thaw frozen leftovers in the refrigerator or microwave, not on the kitchen counter. Reheat them to safe food temperatures until they’re steaming hot.
Tips for managing trouble swallowing
- Choose soft, moist foods.
- Chew your foods well.
If you try following these tips but are still having trouble swallowing or feel like food is getting stuck in your throat, tell your care team. You may need to have a procedure called a dilation to stretch your esophagus to fix this problem. If you need a dilation, your care team will give you more information about what to expect.
Eating at restaurants and social events
Food is the focus of many social events. Remember that portions served at events and restaurants tend to be large. It usually takes some time to get used to eating out at restaurants or attending events like weddings and dinner parties.
- If you finish an appetizer, you may find that you need to take home your entrée.
- If you skip the appetizer, try eating half of the entrée and taking the rest home. You can also share an entrée with a friend.
- You may have to choose either a small soup or a drink as your fluid allowance. Or, you can choose to have just a few sips of both.
- If you want to have dessert after your meal, you may want to have it as your evening snack, along with a 4-ounce drink, 2 ½ to 3 hours later. Read the “6-meal soft diet sample menus” section for examples of how you can plan your meals and snacks.
Resources
MSK support services
Integrative Medicine Service
www.msk.org/integrativemedicine
Our Integrative Medicine Service offers many services to complement (go along with) traditional medical care, including music therapy, mind/body therapies, dance and movement therapy, yoga, and touch therapy. To schedule an appointment for these services, call 646-449-1010.
You can also schedule a consultation with a healthcare provider in the Integrative Medicine Service. They will work with you to come up with a plan for creating a healthy lifestyle and managing side effects. To make an appointment, call 646-608-8550.
Resources for Life After Cancer (RLAC) Program
646-888-8106
At MSK, care does not end after your treatment. The RLAC Program is for patients and their families who have finished treatment.
This program has many services. We offer seminars, workshops, support groups, and counseling on life after treatment. We can also help with insurance and employment issues.
External resources
Academy of Nutrition and Dietetics (AND)
www.eatright.org/public
AND is a professional organization for registered dietitians. The website has information about the latest nutrition guidelines and research and can help you find a dietitian in your area. The academy also publishes The Complete Food and Nutrition Guide, which has over 600 pages of food, nutrition, and health information.
American Institute for Cancer Research
www.aicr.org
800-843-8114
For information on diet and cancer prevention research and education.
FDA Center for Food Safety and Applied Nutrition
www.fda.gov/AboutFDA/CentersOffices/OfficeofFoods/CFSAN/default.htm
For helpful information on food safety.
Clear liquid diet
A clear liquid diet includes only liquids you can see through. These liquids are easy to swallow and digest. Examples are listed in the table below.
While you’re following this diet:
- Don’t eat any solid foods.
- Don’t drink liquids that you can’t see through.
- Drink plenty of liquids besides water, coffee, and tea.
- Don’t drink sugar-free liquids unless you have dumping syndrome.
| Foods and drinks to include | Foods and drinks to avoid | |
|---|---|---|
| Soups |
|
|
| Sweets |
|
|
| Drinks |
|
|
*If soda makes you feel full or gives you gas, try letting it sit out until the bubbles go away or avoid it altogether.
Full liquid diet
A full liquid diet includes all of the things allowed in a clear liquid diet, as well as the foods and drinks below.
| Foods and drinks to include | Foods and drinks to avoid | |
|---|---|---|
| Soups |
|
|
| Dairy |
|
|
| Grains |
|
|
| Nutritional supplements |
|
|
| Miscellaneous |
|
|
Soft diet
A soft diet includes only foods that are physically soft. The goal of a soft diet is to limit the amount of chewing needed to get food into a smooth, easy-to-swallow texture.
Examples of foods and drinks to include in a soft diet are listed in the table below. You can also use the menus in the “6-meal soft diet sample menus” section below.
| Foods and drinks to include | Foods and drinks to avoid | |
|---|---|---|
| Drinks |
|
|
| Breads |
|
|
| Cereals |
|
|
| Soups |
|
|
| Meat and meat substitutes |
|
|
| Milk and dairy |
|
|
| Potatoes and starches |
|
|
| Vegetables |
|
|
| Fruits |
|
|
| Desserts |
|
|
| Oils |
|
|
| Miscellaneous |
|
|
6-meal soft diet sample menus
The sample menus below show a soft diet in 6 small meals. They include 4 ounces of liquid with each meal (to keep you from feeling too full during meals) and 8 ounces of liquid between meals (to keep you well-hydrated). Keep in mind that soup also counts as a liquid.
-
Not all of the menu items are sugar-free. If you have diabetes, high blood sugar, or are having dumping syndrome:
- Use sugar-free or “light” yogurt in place of regular yogurt.
- Limit fruit juices.
- If you drink fruit juices, dilute them with water.
-
Menu items with an asterisk (*) have lactose. If you’re lactose-intolerant:
- Try Lactaid milk, cottage cheese, or ice cream.
- Take Lactaid tablets or drops before having dairy products.
- Choose almond milk, rice milk, or soy milk and non-dairy cheeses.
6-meal soft diet sample menu 1
| Time | Meal | Foods and liquids |
|---|---|---|
| Breakfast |
| |
| Drink |
| |
| Snack |
| |
| Drink |
| |
| Lunch |
| |
| Drink |
| |
| Snack |
| |
| Drink |
| |
| Dinner |
| |
| Drink |
| |
| Snack |
| |
| Drink |
|
6-meal soft diet sample menu 2
| Time | Meal | Foods and liquids |
|---|---|---|
| Breakfast |
| |
| Drink |
| |
| Snack |
| |
| Drink |
| |
| Lunch |
| |
| Drink |
| |
| Snack |
| |
| Drink |
| |
| Dinner |
| |
| Drink |
| |
| Snack |
| |
| Drink |
|
6-meal soft diet sample menu 3
| Time | Meal | Foods and Liquids |
|---|---|---|
| Breakfast |
| |
| Drink |
| |
| Snack |
| |
| Drink |
| |
| Lunch |
| |
| Drink |
| |
| Snack |
| |
| Drink |
| |
| Dinner |
| |
| Drink |
| |
| Snack |
| |
| Drink |
|
6-meal soft diet sample menu 4
| Time | Meal | Foods and Liquids |
|---|---|---|
| Breakfast |
| |
| Drink |
| |
| Snack |
| |
| Drink |
| |
| Lunch |
| |
| Drink |
| |
| Snack |
| |
| Drink |
| |
| Dinner |
| |
| Drink |
| |
| Snack |
| |
| Drink |
|
